International Journal of Scientific & Engineering Research, Volume 6, Issue 5, May-2015 11
ISSN 2229-5518
SONOGRAPHIC EVALUATION OF YOLK SAC
Laly Jose, Nanditha Abdul Latheef
Abstract— Yolk sac is the most important conceptional structure evaluated sonographically in first trimester. Yolk sac can be detected early by transvaginal sonography when the mean gestational sac diameter is 5-6mm. The important benefit of sonographic evaluation of yolk sac is confirmation of intra uterine pregnancy. The present study is aimed at identifying various characteristics of yolk sac in first trimester pregnancy complications by transvaginal ultrasound evaluation. Antenatal patients with bleeding per vagina or abdominal pain or both in first trimester and diagnosed as cases of threatened abortion, missed abortion, incomplete abortion or suspected ectopic gestation were included in the study. Among 133 gestational sacs present by transvaginal sonography, there were yolk sacs in 106 patients (79.7%) and yolk sac was absent in 27 patients (20.3%) with gestational sac MSD >8mm. 27 cases had no yolk sac when the gestational sac diameter was greater than 8mm. Among them 25 cases with the absence of yolk sac and fetal pole when the MSD >8mm ended up in complications. However there were 2 cases with no yolk sac but a normal appearing gestational sac and fetal pole with good cardiac activity till 10 to 11 weeks which were subsequently lost for further follow up. The association between the presence of the yolk sac and the final ultrasound diagnosis was significant (p<0.001). Assessment of yolk sac should be part of complete first trimester sonographic examination. An abnormality in sonographic appearance of yolk sac can predict subsequent embryonic health or abnormalities. There for accurate recognition of normal and abnormal sonographic findings related to yolk sac can be used to anticipate the course of pregnancy.
Index Terms— Embryonic health, Pregnancy, Sonography, Transvaginal ultrasound, Yolk sac.
—————————— ——————————
olk sac is the most important conceptional structure eval- uated sonographically in first trimester. Yolk sac can be detected early by transvaginal sonography when the mean gestational sac diameter is 5-6mm. The important benefit of sonographic evaluation of yolk sac is confirmation of intra uterine pregnancy [1, 2]. It has been hypothesized that sonographic features related to shape, size and internal struc- ture of yolk sac can be associated with gestational outcome [3]. Normally the yolk sac appears as circular structure with an- echoic center surrounded by a uniform well defined echo- genic wall. Usually inner diameter of yolk sac measures 3 mm – 5 mm. The yolk sac size progressively increases from beginning of fifth week of gestation to end of tenth week of
gestation. Afterwards yolk sac decreases gradually in size [4].
The present study is aimed at identifying various
characteristics of yolk sac in first trimester pregnancy compli-
cations by transvaginal ultrasound evaluation.
Antenatal patients who presented to causality or Ob- stetrics unit of Karakonam Medical college either with bleed- ing per vagina or abdominal pain or both in first trimester and diagnosed as cases of threatened abortion, missed abor- tion, incomplete abortion or suspected ectopic gestation for a period of 1 ½ years from August 2010 - January 2012 were
————————————————
• Dr. Laly Jose, Professor of Radiodiagnosis, SM CSI Medical College, Karakonam P O, Thiruvananthapuram- 695504
• Dr. Nanditha Abdul Latheef, Associate professor of Radiodiagnosis, SM CSI Medical College, Karakonam P O, Thiruvananthapuram- 695504
All first trimester pregnancies with bleeding per vagina and or abdominal pain who were referred for so- nography from Dept. of Obstetrics and Gynecology de- partment of SMI CSI Medical College, Karakonam. Exclusion Criteria
Cases where patients were not willing for transvaginal
Ultrasound.
Ethical clearance was obtained from institution review board. The study was done using Siemens Sonoline G 50 transabdominal USS using 3 to 5 MHz convex transducer followed by transvaginal uss using 5 -10 MHz endovaginal
transducer. Patient was followed up as indicated or upto
20 weeks of gestation. Detailed evaluation of yolk sac which
included size, shape, echogenicity and presence of calcification
was performed.
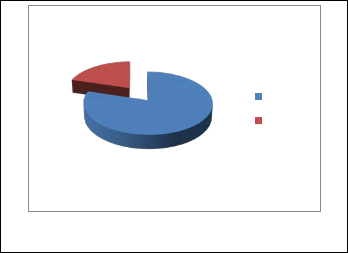
20.3
Present
Absent
79.7
included in the study.
Fig. 1 Percentage distribution of the sample according to presence of yolk sac
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 5, May-2015 12
ISSN 2229-5518

Diagram shows that in the total 133 gestational sacs present by transvaginal sonography, there were yolk sacs in
106 patients (79.7%) and yolk sac was absent in 27 patients
(20.3%) with gestational sac MSD >8mm.
Fig. 3 Echogenic yolk sac in a case of missed abortion with fetal pole showing no cardiac activity

Fig.2 Normal yolk sac at 6 weeks of gestation
TABLE 1
ASSOCIATION BETWEEN THE PRESENCE OF THE YOLK SAC AND FINAL OUTCOME ON FOLLOW UP WITH MSD >8MM
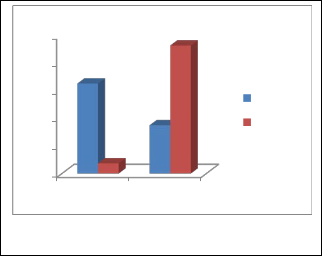
Fig. 4 Calcified yolk sac in a case of missed abortion
100
80
60
40
20
0
65.1
7.41
34.9
92.6
Normal
Abnormal
Yes No
Fig. 5 Distribution of final outcome of pregnancy on follow- up according to the yolk sac presence
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 5, May-2015 13
ISSN 2229-5518
27 cases had no yolk sac when the gestational sac diameter was greater than 8mm. Among them 25 cases with the absence of yolk sac and fetal pole when the MSD >8mm ended up in complications.
However there were 2 cases which no yolk sac but a normal appearing gestational sac and fetal pole with good cardiac activity till 10 to 11 weeks which were subsequently lost for further follow up.
The association between the presence of the yolk sac and the final ultrasound diagnosis was significant (p<0.001).
TABLE 2
PERCENTAGE DISTRIBUTION OF THE SAMPLE ACCORDING TO AB- NORMALITY OF YOLK SAC
TABLE 3
ASSOCIATION BETWEEN ABNORMALITY OF THE YOLK SAC AND FINAL OUTCOME OF PREGNANCY ON FOLLOW UP
69.8
70
60
50
40
30
20
10
0
30.2
30.7
69.3
Normal
Abnormal
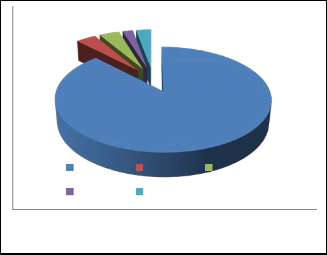
3.7 3.7 1.9 2.8
Normal
Appearance
Abnormal
Appearane
Figure 7 Distribution of final outcome according to follow up
according to abnormality in appearance on yolk sac
87.7
Normal Echogenic Small
Large Calcified
Figure 6 Showing percentage distribution of sample according to appearance of yolk sac
Figure 6 shows that about 88% of the visualized yolk sac were normal, in 3.7% it was echogenic, in 4% small, 1.9% large and 2.8% calcified. From this it was seen that most of the subjects had a normal yolk sac.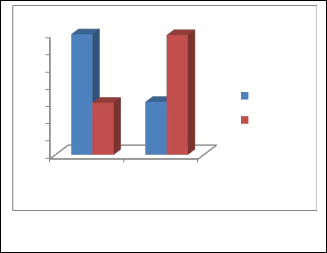
Table 3 and figure 7 shows 69.3% of patients having abnormally appearing yolk sac on ultrasound examination ended up in complications whereas only 30.2% of patients having normal appearing yolk sac had complications. This association was seen to be statistically significant.
In 106 patients (79.7%) the yolk sac was present and in 27 patients (20.3%) it was not present. 25 cases with absence of yolk sac when the MSD>8mm by TVS and which had no fetal pole among the total 27 cases having no yolk sac had an abnormal outcome on follow up.
Cho FN et al [5] conducted a study in which Trans- vaginal ultrasonography was performed in 111 normal single- ton pregnancies, 25 anembryonic gestations, and 18 missed abortions. The relationship between yolk sac and gestational sacs in normal pregnancies was depicted. The ultrasound find- ings regarding yolk sac in cases of pregnancy loss were also recorded. It was seen in this study that as the pregnancy
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 5, May-2015 14
ISSN 2229-5518
matures, a yolk sac becomes visible on transvaginal scan by
8mm MSD or by 20mm MSD on transabdominal scan.
According to Varela et al [6] in transvaginal Sonography,
absence of yolk sac in presence of an embryo is always
abnormal and in general is associated with subsequent fetal
loss.
In about 88% the yolk sac was normal, in 3.7% it was echogenic, in 3.7% small, 1.9% large and 2.8% calcified. From this it was seen that most of the subjects had a normal yolk sac. Among the abnormal yolk sacs 69.3% went into complications whereas 30.2% only went into complications among the pregnant women who had normal yolk sac. This association was seen to be statistically significant. Among the
4 cases having a small yolk sac (<2mm), 3 were seen to continue as normal pregnancy. Only one went into spontaneous expulsion. The 3 patients with calcified yolk sac were diagnosed to have missed abortion and went into spontaneous expulsion.
An earlier study [7] with certain limitations suggests that yolk sac diameter of 2mm or less may be associated with adverse outcome in pregnancy with gestational age of
8-12weeks. Echogenic yolk sacs were mostly seen in an embryonic gestation (3 out of 4). A single case of missed abortion was seen with an echogenic yolk sac. Also among the large yolk sacs (>5mm), one case continued as normal pregnancy. The other case went into spontaneous expulsion even in the presence of an embryo with good cardiac activity.
In Cho FN et al [5] study also it was seen that the largest yolk sac in viable pregnancies was 8.1mm. In anembryonic gestations an absent yolk sac, an irregular shaped yolk sac and a relatively large yolk sac was seen (>95% upper confidence limits, in 11 cases). A very large yolk sac may exist in normal pregnancy as was seen in our study also. Thus they concluded that when embryonic heartbeats exist, the poor quality and early regression of a yolk sac are more specific than the large size of a yolk sac in predicting pregnancy loss. When an embryo is undetectable, a relatively large yolk sac, even of normal shape, may be an indicator of miscarriage. According to Berdabl et al [8] a yolk sac diameter of greater than 5mm is associated with increased risk of spontaneous abortion.
According to Sinan Tan et al [9] assessment of yolk
sac should be part of a complete first trimester sonographic
examination. An abnormality in the sonographic appearance
of a yolk sac can predict subsequent embryonic death or ab-
normalities.
Assessment of yolk sac should be part of complete first trimester sonographic examination. An abnormality in sonographic appearance of yolk sac can predict subsequent embryonic health or abnormalities. There for accurate recognition of normal and abnormal sonographic findings related to yolk sac can be used to anticipate the course of pregnancy.
[1] Carol MR, Stephane RW, Charboneau IW, Debord FL; Diagnostic ultrasound
Philadelphia, Elsevier Mosby -2011.
[2] Jauniaur E, Johns J, Burton GJ. The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound obstet. Gynaecol. 2005
June 25(6): 613-24.
[3] Tans, Ipek, Pektas MK, Aoifogu, Teber MA, Karaglanoglu. Irregular sac shape. Is it really associated with increased risk of spontaneous abortion. Ul- trasound. Med. 2011; 30 : 31-35.
[4] Nyberg DA, Mack LA, Horvey D, Wang K. Value of yolk sac in evaluating early pregnancy. J. Ultrasound Med. 1988; 7:129-133.
[5] Cho FN, Chen SN, Tai MH, Yang TL. The quality and size of yolk sac in early pregnancy loss. Aust N Z J Obstet Gynaeco. 2006 Oct. 46(5):413-8.
[6] Varelas FK, Prapas NM. Liang RI, Prapas IM, Makedas GA. Yolk sac size and embryonic heart rate as prognostic factors of first trimester pregnancy out- come. Europ. J. Obstet. Gyanecol. Reprod. 2008; 138: 10-13.
[7] Green JJ, Hobbins JC. Abdominal ultrasound examination of first trimester fetus: Am J Obstet. Gyanecol. 1988; 159: 155-167.
[8] Berdabl DM, Blaine J, Van Voorbis B, Dokras A. Detection of enlarged yolk sac on early ultrasound is associated with adverse pregnancy outcomes. Fertli. Steril 2010; 94 : 1535-37.
[9] Sinan Tan MD, Mine Kanat Dektas, Halil Arslan; Sonographic evaluation of yolk sac. Journal of ultrasound in medicine. January, 2012 ; Vol. 31: 87-95.
IJSER © 2015 http://www.ijser.org