International Journal of Scientific & Engineering Research, Volume 5, Issue 12, December-2014 514
ISSN 2229-5518
Polycystic Ovary Syndrome (PCOS)
Mehak Joshi
Abstract— In this term paper, the emphasis is given on Polycystic Ovary Syndrome (PCOS) and infertility problem due to it. PCOS is one of the common endocrine disorder among women of reproductive age. In this condition, what basically happens is the ovaries contain multiple cysts or follicles that develop but do not grow to maturity or produce eggs that are capable of being fertilized. Due to this problem of lack of ovulation, women with PCOS problem also suffer from major problem of infertility. In present scenario, researchers have yet not found the exact cause of PCOS but recent studies and present researches that are going on have come out with some causes like hormonal imbalance, resistance to insulin, genetic factors etc. Due to imbalance in hormones, women have irregular menstrual periods. The two hormones namely, estrogen and progesterone, responsible for woman’s ovaries to release eggs, are at lower level than normal level and then they lack follicle maturation. The result of it is that there is a filled cyst in the ovaries in which follicle mature to enlarge, forming cysts and hence polycystic ovary. Several physical symptoms appear in woman suffering from PCOS like irregular periods, hirutism etc. During the process of diagnosis, the patient is asked about his medical history and doctor will perform some basic tests like pelvic exam, ultrasound, blood test, and screening laboratory tests etc. Till present, there is no perfect cure for treatment of PCOS. But to reduce the symptoms and the problem of infertility associated with it, researchers have come up with certain treatments. Metformin therapy is advised by doctors to stimulate continuation of normal, ovulatory menstrual cycles. LH-releasing hormone (LHRH) analogs and Clomiphene citrate are the medicines which will help in getting pregnant and help the ovaries to grow follicles and release eggs.
Index Terms— Acne, Cysts, Hirutism, Hormonal imbalance, Infertility, Irregular periods, Obesity
—————————— ——————————
1 INTRODUCTION
olycystic Ovary Syndrome (PCOS) is one of most common hormonal disorder among the women of reproductive age. In this condition, a woman’s ovaries are generally
bigger than normal size. Basically, it is a condition in which there is an imbalance of female sex hormones which lead to infrequent menstrual cycles. (Kirtly Jones, 2012)
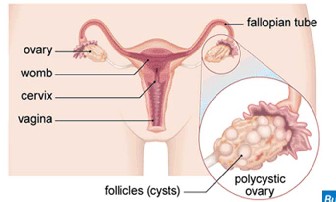
Profoundly, polycystic means the ovaries have multiple cysts or follicles that hardly grow to maturity or produce eggs that are capable of being fertilized. PCOS is one of the poorly described endocrine system disorder with a complicated pathophysiology that has generated significant scientific debate (Patrice Burgess, 2010).The most important point to be clear when talking about the prevalence in the population is difference between the definitions that are usually used. Polycystic ovaries should not be muddled with the term polycystic ovary syndrome. Polycystic Ovary Syndrome (PCOS) refers to presence of multiple cysts in an ovary of a woman with specific group of symptoms which commonly includes hirutism, amenorrhea, oligoamenorrhea, acne etc. (Legro RS et al, September 2012). However, a woman may be diagnosed with polycystic ovaries during ultrasound examination for some different reasons, who have none of the above mentioned symptoms, implies she do not have the syndrome – means do not have the symptoms associated with PCOS. (Dimanti-Kandarakis E et al, August 2006).
PCOS was first originally reported in 1935 by Irving F.Stein and Michael L. Leventhal when they first presented their research paper at the Central Association of Obstetricians and Gynecologists (Teede H et al, 2010). In their classical observation, they described a group of women with amenorrhea, infertility, hirutism and enlarged polycystic
————————————————
• Mehak Joshi is currently pursuing bachelors degree program in medical Biotechnology in Amity University, India, PH-9873132502. E-mail: mehakbutterfly@gmail.com
ovaries with thickened tunica. Since, PCOS was reported by Stein and Leventhal; it is also called Stein-Leventhal Syndrome. PCOS is one of the most common causes of infertility and cause enormous influence on a woman’s quality of life. (Brennan K et al, 2010)
2 CAUSES
At present, doctors and researchers are not sure what basically cause PCOS, but recent studies and present researches that are going on suggest that PCOS is result of number of both genetic (inherited) as well as environmental factors. Researchers are not clearly able to find the role of genetics or gene mutations in PCOS (Silfin ME st al, 2001). However, scientists are quite successful in finding the proposed causes of PCOS which are numerous. They are briefly listed below:-
2.1 Hormonal Imbalance
PCOS is mainly caused by changes in hormone levels that make difficult for the ovaries to release mature eggs. The two hormones mainly estrogen and progesterone, known as “female hormones” are the hormones that are responsible for the woman’s ovaries to release eggs. When these hormones which trigger ovulation are not at right level that is they are at lower than normal levels of estrogen, and then they lack follicle maturation (Ducluzeau PH, 2003). The result of it is that there are filled cysts in the ovaries in which follicle grow and mature to enlarge, forming cysts. Also, in women with PCOS there is increased production of androgen by the adrenal gland during puberty which is responsible for hirutism (excessive growth of facial or body hair in women), acne production etc.
2.2 Resistance to Insulin
Insulin is a hormone which helps in controlling the amount of sugar in the blood. This hormone secreted by the pancreas,
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 12, December-2014 515
ISSN 2229-5518

helps in moving glucose from blood into cells; where it is broken down to give out energy. Insulin resistance implies that the body’s tissues are resistant to the effects of insulin (Sams et al, 2012). Therefore, the body has to produce extra insulin to compensate. PCOS is associated with insulin resistance as well as defects in insulin. High levels of insulin in the body cause the ovaries to produce too much testosterone hormone, which interferes with the follicle development and prevent normal ovulation (Wilcox AJ, 1998).
2.3 Genetics
Polycystic ovary syndrome (PCOS) sometimes runs in
families. If any relatives, such as your mother or sister, have PCOS then the risk of you developing it is often increased. This suggests there may be a genetic link to PCOS, although specific genes associated with the condition have not yet been identified.
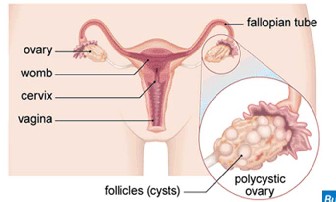
Fig. 1. An Ovary Affected By Polycystic Ovary Syndrome
3 SYMPTONS
Symptoms of PCOS typically start soon after a woman begins to menstruate. The category and seriousness of symptoms varies from person. The following common symptoms are as follows:-
3.1 Irregular periods
The most common symptom is having irregular periods or no periods for a prolonged time.
3.2 Obesity
Weight gain, being overweight and problem in losing weight. Women with PCOS had a great risk of overweight and obesity (Norman RJ et al, 4th July 2012)
3.3 Hirutism
Due to increase of male hormones, there is an excessive thick hair growth on face, chest, especially near areola region of mammary glands, neck, buttocks, lower abdomen etc.
Fig. 2. Problem of Hirutism
3.4 Hair Loss
There is thinning of hair or hair loss from the head.
3.5 Infertility
Due to excessive production of androgen, it leads to irregular ovulation, which women experience as irregular or absent menstrual periods. Due to this major problem with ovulation, women with PCOS have major difficulty in becoming pregnant. (Niven Todd, MD, FACOG, June 2012)
3.6 Acanthosis nigricans
It is darkening and thickening of some areas of the skin, especially around neck, underarms and groin

Fig. 3. Problem of Acanthosis nigricans
3.7 Cysts
Multiple tiny cysts, women with PCOS have a large number of cysts which is visible by ultrasound in their ovaries.
4 DIAGNOSIS
Polycystic ovarian syndrome (PCOS) is a highly common disorder affecting 4% to 12% of women of reproductive age (knochenhauer ES et al, 1998). Although being diverse in nature, the characteristic features of the disease are hyperandrogenism and chronic anovulation.
The diagnosis of PCOS is totally based on hyperandrogenism or chronic anovulation in the absence of specific pituitary and adrenal disease. The differential diagnosis of PCOS is listed below table 1.1 along with the tests needed to adequately assess for these possibilities.
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 12, December-2014 516
ISSN 2229-5518
A careful history and physical examination, looking for other signs of those defects that may not be a part of PCOS, must be performed. Symptoms of cold intolerance, dry skin, and increased fatigue (among others) may signify hypothyroidism, as would the presence of a goiter. Galactorrhea may or may not be present in women with hyperprolactinemia. Signs of virilization signify more significantly elevated androgen levels than those seen in PCOS and may indicate an ovarian or adrenal tumor. Patients with Cushing's syndrome may be more apt to have high blood pressure, purple abdominal striae, prominent dorsal cervical fat pads, and a rounded, swollen face ( Ducluzeau PH, 2003)
Late-onset congenital adrenal hyperplasia, even though relatively rare, deserves mention as it can mimic PCOS in all regards clinically. Congenital adrenal hyperplasia is due to one of a variety of enzymatic defects in adrenal steroid genesis (which leads to increased levels of precursor hormones that have androgenic properties). The classic forms of these disorders involve complete enzymatic defects and present in newborn girls as ambiguous genitalia. More recently partial enzymatic defects in these same pathways have been shown to not present until menarche and then with irregular menses and hirutism mimicking PCOS. Measurement of the hormone preceding the enzymatic block is used to definitively diagnose these disorders. The most common form of late-onset congenital adrenal hyperplasia is due to 21-hydroxylase deficiency and, as such, is often the only type tested for in the differential diagnosis of PCOS. (Conway GS, 1989)
There's no specific test to definitively diagnose polycystic ovary syndrome. The diagnosis is one of the rejections, which means that doctor considers all of your indications and symptoms and then rules out other possible disorders (Bracero N, 2001)
During the process of diagnosis, the patient will be asked about his medical history, including menstrual periods, changes in weight, and other symptoms. The doctor will perform first some basic tests. They are as follows:-
4.1 Pelvic Exam
During this test, the doctor will visually and manually inspect the reproductive organs for signs of masses, growth or any other abnormalities.
4.2 Physical Exam
The doctor will note several key pieces of information; for instance signs of hirutism, darkening areas around neck and under armpits etc
4.3 Blood Test
The blood test will be done to measure the level of several hormones eliminate possible causes of menstrual problems or excess androgen that mimic PCOS. Additional blood testing may also be done which include fasting cholesterol and levels of triglyceride and a glucose tolerance test, in which glucose levels are measured.
4.4 Ultrasound Scan
An ultrasound scan of lower abdomen is done which show ovaries and thickness of the lining of uterus. If multiple small
cysts are seen in ovaries, then there are possible chances of
PCOS.
Presence of cysts in ovaries is not specific for PCOS. The
number of follicles and volume of ovary both are important in
ultrasound evaluation.
Apart from these above mentioned basic tests, screening
laboratory studies for women considered of having PCOS are as follows:-
1. Total and free testosterone levels
2. Low dose dexamathasone suppression test
3. Insulin level
4. Thyroid function test
5. Serum prolactin test
6. Free androgen index
Perhaps this ‘clinical’ consensus should be different than that
used in the research setting. An extremely practical proposal
has recently been put forth for the diagnosis of PCOS by
Homburg (Homburg R, 2002). In this proposal any one of four
classic symptoms of PCOS (menstrual disturbance, hirutism, acne problem or anovulatory infertility) should lead to an ultrasound evaluation of the ovaries. If polycystic ovaries are found, the diagnosis is confirmed. If the ovarian morphology
is normal, then biochemical testing is undertaken.
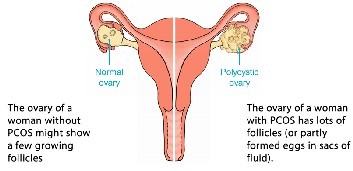
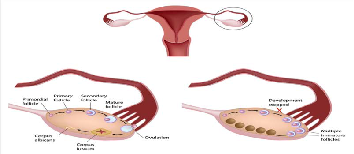
5 WORKING OF NORMAL AND POLYCYTIC OVARY
5.1 Normal Ovary
Ovulation occurs when one or more follicles are released from one of the ovaries. This occurs towards the end of the time when one is fertile between periods. Every month, between 15 and 20 eggs grow inside ovaries. The egg which is ripened is released and move into one of the fallopian tubes. Almost about 14 -15 days after ovulation, the woman will have periods if she is not pregnant. (Richard Sherbahn, 2010)
5.2 Polycytic Ovary
The chief difference between normal ovaries and polycystic ovaries is that while the polycystic ovaries contain numerous antral follicles with eggs inside them, the follicles do not develop and grow properly, so there is no ovulation in women with PCOS. Due to this major difficulty of no ovulation, or irregular ovulation, women with PCOS suffer from problem of infertility (Silfin ME, 2001)
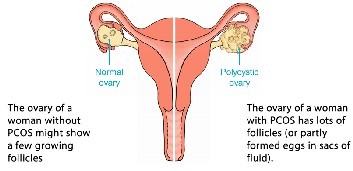
Fig. 4. Growing follicles in normal ovary and immature eggs in polycystic ovary
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 12, December-2014 517
ISSN 2229-5518
6 INFERTILITY RATE DUE TO PCOS
The infertility rate of women with polycystic ovaries is really very high. These women usually do not ovulate and have difficulty in getting pregnant and also require proper treatment to improve the possibilities of getting pregnant. Some women with PCOS will ovulate occasionally and others do not ovulate ever. In order to conceive, sperm must find a mature egg and fertilize it (Franks NS, 1995) The low or varied levels of follicle stimulating hormone (FSH) allow numerous follicles to develop but without ever maturing any one follicle. Thus, many follicles are present inside ovaries and once they become ataractic they will form cysts, hence they are called polycystic ovary. Since these follicles do not mature and do not release egg, lack of ovulation or anovulation is seen which most likely cause is of infertility (Palson DW et al, 1998)
metabolism, and anovulation (when your ovaries do not release an egg).
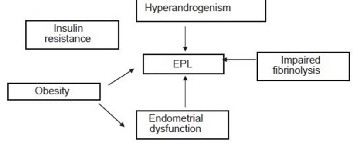
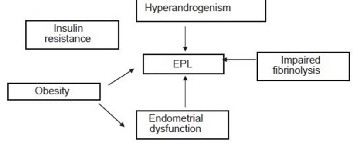
7 EARLY PREGNANCY LOSS
In women suffering from PCOS, the first trimester miscarriage rate is high as 30% to 50% (Homburg R et al, 1988). The women are at a great risk of early pregnancy loss. The probable pathophysiology for early pregnancy loss can be explained by following chart:-
a
Chart 1. PATHOPHYSIOLOGY OF EARLY PREGNANCY LOSS
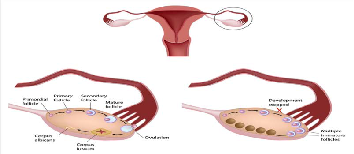
Fig. 5. Difference between Normal and Polycystic Ovary
The reproductive disturbances are more common in obese women irrespective of diagnosis of PCOS. Generally, obese women are more likely to have an irregular menstrual period which leads to lack of ovulation and results in infertility. In spite of the higher prevalence of reproductive disorders in obese women, the majority of obese women does not develop hyperandrogemia and do not have PCOS (Jonards S 2003). Weight gain due to PCOS leads to imbalance of hormones which leads to increased androgen production which results in problem of hirutism, deepening of voice, decrease in breast size etc. Also “female hormones”, testosterone and progesterone are at levels lower than normal level of estrogen in polycystic woman, and then they lack follicle maturation which leads to irregular menstrual periods and results in infertility (Pasquali R, 1993).
Insulin is secreted by the pancreas in order to digest sugar and convert it to energy. Women with PCOS have insulin resistance, which means that in spite of the presence of insulin, sugar is not being digested properly. This ultimately results in the conversion of sugar to fat, obesity, a disturbed sugar
Hypofibrinolysis because of increased plasminogen activation inhibitor might also be an independent risk factor for early pregnancy loss in PCOS (Jakubowicz et al, 2002). Finally, insulin resistance the chief pathophysiology of PCOS has been proposed to play an essential role in the development of spontaneous abortion ( Gluek J et al, 1999).
High androgen levels and high insulin levels have detrimental effect on endometrial development and increased androgen levels also decrease oocyte quality and embryo viability (Boklage CE, 1990).
8 TREATMENT FOR INFERTILITY DUE TO PCOS
Women suffering from PCOS are at great danger of early pregnancy loss, infertility and reproductive problems. Earlier no special fertility treatment was available and frequent miscarriage used to occur. But there is good news for PCOS patients as with advanced researches and studies, researchers have come up with various fertility treatments with high success rate. Majority of women suffering from Polycystic Ovary Syndrome will now be able to have baby with advance fertility treatments.
8.1 Natural Treatment
8.1.1 Weight reduction
The very first treatment doctor would advice to his patients to lose weight. This treatment itself is natural for an obese women suffering from PCOS weight reduction is very first step to increase chances of getting pregnant. Losing weight will balance the hormones, improve ovulatory function, regulate menstrual cycle, which will make easier to conceive and have safer pregnancy. Weight reduction has also shown to reduce hyperinsulinemia and hyperandrogenism (Conway GS, 1989)
8.1.2 PCOS Diet
Eating a specific PCOS fertility diet is one of the best things the patients can do to prove the chances of pregnancy.
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 12, December-2014 518
ISSN 2229-5518
Majority of women suffering from PCOS have high insulin resistance. High insulin resistance increases the body’s insulin levels which greatly affects normal ovulation, limiting the maturation process of released egg. This results in infertility. The PCOS diet:-
1. Improves uterus environment for healthy conception.
2. Increases the rate of voluntary ovulation
3. Decreases the chances of miscarriage
4. Avoid diabetes
8.2 Ovule Induction
Infertility treatment caused due to PCOS is directed at preparing the woman to ovulate. This process is done by doctors and is called “induction of ovule” (). Ovule induction includes the use of medicines to stimulate development of one or mature follicles in the ovaries of women who have problem ovulating and infertility. The medications are as follows:-
8.2.1 Clomphine Citrate (Clomid)
It is also an oral medicine often given to induce ovulation in women who do not develop and release a egg on their own (Jakubowicz DJ, 2002).
8.2.2 Metformin
Basically it is a diabetes medicine for treating ovulation problems. Studies have shown that taking Metformin therapy continued throughout pregnancy have shown to reduce the danger of early pregnancy loss. Also, Metformin if taken with low dose of Clomiphene have shown great results for obese women. Also, taking Metformin throughout pregnancy has shown no birth defects (Glueck CJ, 2001). The medication Metformin has also proved to be in improving rates of fertilization and pregnancy in women with PCOS undergoing in vitro fertilization (IVF).
8.2.3 Femara
Femara (letrozole) is an oral medicine which can be potent fertility treatment for women with ovulation abnormalities, or for those with infertility. When the enzyme aromatase is inhibited by the letrozole medicine, levels of estrogen are suppressed in young women. This results in the brain and pituitary gland increasing the output of FSH (follicle stimulating hormone). In women that have polycystic ovary syndrome, the increase in FSH hormone can result in development of a mature follicle in the ovary and ovulation of an egg. Doctors call this process "induction of ovulation".
8.2.4 Injectables for fertility
Injectable FSH hormone products are frequently mentioned to as injectable gonadotropins or "injectables". Fertility patients with PCOS have commonly tried treatment with oral medications as a first-line therapy, and if that is not successful, moving on to injections is another option. US brand names for injectables include Follistim, Gonal-F, Repronex, Bravelle, and Menopur (Ducluzeau PH, 2003)
6.3 When are Injectables used in women with PCOS?
When oral medicine treatments, such as Clomid for PCOS or Femara for PCOS fail to result in a viable pregnancy, it used to be routine that the upcoming step was shots for infertility
However, because of the great risk for multiple births, particularly the danger of triplets and higher, injectable for PCOS is being used less frequently. When injectable are used to activate ovulation in women with polycystic ovaries it is often very hard to get only 1 or 2 follicles to develop. Commonly there are several follicles at or near a mature size by the end of the ovarian activation process. Multiple follicles close to mature size at ovulation time give a greater risk for multiple pregnancies. Because of these risks, and because IVF has high success rates, many couples and infertility specialists now directly move to IVF if clomiphene treatment is unsuccessful.
6.4 Procedure for using Injectables for Pregnancy with
PCOS:-
These medications are usually given by subcutaneous injections on a regular basis. The injections are commenced early in the menstrual cycle, which is frequently induced with medicin. Daily injections persist for approximately 7 to 14 days with the doctor adjusting the dose in order to get 1 (or a few) follicles to grow. When one (or more) matures size follicles are seen in the ovaries with ultrasound, an injection of HCG is given which stimulates ovulation to occur about 37 to 40 hours later (Bulun SE, Adashi EY, 2011).
7 CONVENTIONALTREATMENT FOR PCOS
7.1 Control of Irregular Menses
This basic feature of PCOS can be both a nuisance and a significant health risk to patients. Irregular menses can be embarrassing because of unpredictability and painful because the infrequent occurrence often leads to increased cramping with the heavier flow. Infrequent menstrual cycles also carry a
3-fold increased risk of endometrial carcinoma. In general, four menses per year are required to control this increased risk. To regulate your menstrual cycle, your doctor may recommend combination birth control pills — pills that contain both estrogen and progestin. These birth control pills decrease androgen production and give your body a break from the effects of continuous estrogen, lowering your risk of endometrial cancer and correcting abnormal bleeding. As an alternative to birth control pills, you might use a skin patch or vaginal ring that contains a combination of estrogen and progestin. During the time that you take this medication to relieve your symptoms, you won't be able to conceive (Bulur SE,2011)
If one is not a good candidate for combination birth control pills, an alternative approach is to take progesterone for 10 to
14 days every one to two months. This type of progesterone therapy regulates one’s periods and offers protection against endometrial cancer, but it doesn't improve androgen levels and it won't prevent pregnancy. The progestin-only minipill or progestin-containing intrauterine device is better choices if one also wishes to avoid pregnancy.
7.2 Hirutism Treatment
Doctor may recommend birth control pills to decrease
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 12, December-2014 519
ISSN 2229-5518
androgen production, or another medication called spironolactone (Aldactone) that blocks the effects of androgens on the skin. Because spironolactone can cause birth defects, effective contraception is required when using the medicine and it's not recommended one is pregnant or planning to become pregnant. Eflornithine (Vaniqa) is another medication possibility; the cream slows facial hair growth in women. Excess testosterone production is predominantly ovarian in nature and is caused by both increased luteinizing hormone (LH) stimulation from the pituitary and the effect of hyperinsulinemia at the ovary (Gluek CJ et al, 2001). There are several anti-androgens available, but only spironolactone will be discussed further since many of the others have poor side effect profiles, are expensive, or are unavailable in the market. Spironolactone is an aldosterone antagonist that was initially introduced as an antihypertensive agent. Combined contraceptive pills that contain drospirenone, such as Yasmin, suppress androgens (male sex hormones). This means they can be used to treat hirsutism. Drospirenone is also anti- androgenic, which means it prevents the androgens from working, thereby preventing excess hair growth.Combined oral contraceptive pills are usually the first choice of treatment in premenopausal women, and are particularly useful if long- term treatment is necessary (Boklage CE, 1990)
7.3 Acne Treatment
This condition results from the formation of comedones, due to sebum accumulation, along with desquamated follicular epithelial cells, which allows colonization by the bacterium, Propionibacterium acnes (P. acnes).Androgens may worsen acne formation by increasing sebum production within the pilosebaceous unit. Many PCOS women with acne exhibit facial lesions and up to 50% of individuals demonstrate lesions on the neck, chest, and upper back. Flutamide is a non- steroidal androgen receptor antagonist indicated for the treatment of prostate cancer and has been found to be effective for treating hirsutism. Flutamide may be used for the treatment of mild to moderate acne. It should be used at low doses; 62.5 mg or 125 mg per day have been shown to be effective (Barbieri RL, et al., 2005).In hirsute women with acne who were treated with Oral contraceptive pills, the addition of flutamide was significantly more effective than spironolactone.
8 LAPAROSCOPIC OVARIAN DRILLING (OVARIAN
DIATHERMY) FOR PCOS
Laparoscopic ovarian drilling is a surgical treatment that can trigger ovulation in women who have polycystic ovary syndrome (PCOS). Electrocautery or a laser is used to destroy parts of the ovaries. This surgery is not commonly used. But it can be an option for women who are still not ovulating after losing weight and trying fertility medicines.
Ovarian drilling is usually done through a small incision (laparoscopy), with general anesthesia. The surgeon makes a small cut (incision) in the abdomen at the belly button. The surgeon then places a tube to inflate the abdomen with a small amount of carbon dioxide gas so that he or she can insert the viewing instrument (laparoscope) without damage to the
internal organs. The surgeon looks through the laparoscope at the internal organs. Surgical instruments may be inserted through the same incision or other small incisions in the pelvic area. Because the incisions are so small, laparoscopy is often called "Band-Aid surgery."

Fig. 6. Ovarian drilling by Laparoscopy
8.1 Why It Is Done?
Ovarian drilling is sometimes used for women with PCOS who are still not ovulating after trying weight loss and fertility medicine. Destroying part of the ovaries may restore regular ovulation cycles.
8.2 How Well It Works?
For women who do not respond to treatment with medicine, such as clomiphene, about 50% of them may be able to become pregnant after they have ovarian drilling surgery.
8.3 Risks of Ovarian Drilling
There are some risks associated with ovarian drilling, as outlined below.
1. There is a minimal risk of bleeding, infection and death, like with most surgeries.
2. Risks of anesthesia are also present.
3. Tools used during the procedure could damage your
internal organs.
4. The doctor could destroy too much of the ovary. This
could cause your egg supply to diminish at a young age, sending you into early menopause.
5. Scar tissue can form between the ovaries and
fallopian tubes. This can make conception even more
difficult after the surgery. Due to these factors,
ovarian drilling is only advised for women whose
fertility problems stem from PCOS. (Jakubowicz, et al.
2002).
9 CONCLUSION
From this endocrine disorder of Polycystic Ovary Syndrome (PCOS), I conclude that PCOS is one of the most common disorders affecting women of reproductive age. As a syndrome, it has multiple elements, which include reproductive, metabolic, and cardiovascular, with long-term
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 12, December-2014 520
ISSN 2229-5518
health concerns that cross the life span. PCOS is a disorder in which imbalance in hormones give rise to multiple problems like diabetes, hirutism, acne, infertility, etc. Genetic variation of the PCOS phenotype does exist and visible to be linked to differing genetic and environmental tendency to metabolic and hormonal disorder. This aspect needs acknowledgement in routine clinical practice as well as in PCOS-related research. The implications of genetic variation on screening and diagnosis, management consideration and response to treatment must be taken into consideration when managing women from distinct ethnic backgrounds, as well as in developing management guidelines. Long-term follow-up studies are prescribed to explain relevant issues with higher accuracy. Though the researchers have come up with various fertility treatments but still specific treatment till date is not known. Instead of multiple treatments to reduce symptoms of the disease and providing different medicines for different treatments, research should focus on single medication to cure all the symptoms of the disease. Fertility treatments which are oral medications to induce ovulation are given to patients though helps the patient in getting pregnant but on the other hand have numerous side effects like hair loss, breast tenderness, breast pain, abdominal pain, nausea, swelling in hands and headache, skin rash and itching, insomnia and depression, migraine etc. Even birth control pills given to have regular periods have same side effects. In the end, I would end up here with conclusion that research should be done on specific treatment for PCOS as if this disorder not treated properly could lead various cancers and others serious diseases like diabetes, etc.
REFERENCES
[1] Hoffman BL, et al. Williams Gynecology. 2nd ed. New York, N.Y.: The McGraw-Hill Companies; 20. Accessed June 2, 2014.
[2] Barbieri RL, et al. Clinical manifestations of polycystic ovary syndrome in adults. http://www.uptodate.com/home. Accessed June 4, 2014.
[3] Barbieri RL, et al. Treatment of polycystic ovary syndrome in adults.
http://www.uptodate.com/home. Accessed June 4, 2014.
[4] AskMayoExpert. What is the initial therapy recommended for polycystic ovary syndrome (PCOS)? Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2013.
[5] Polycystic ovary syndrome (PCOS) fact sheet. Womenshealth.gov. http://www.womenshealth.gov/publications/our-
publications/fact-sheet/polycystic-ovary-syndrome.html. Accessed
June 4, 2014.
[6] Sirmans SM, et al. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clinical Epidemiology. 2014;6:1.
[7] Legro RS, et al. Diagnosis and treatment of polycystic ovary syndrome: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology and Metabolism. 2013;98:4565.
[8] Strauss JF, et al. Yen & Jaffe's Reproductive Endocrinology. 7th ed.
Philadelphia, Pa. Elsevier Saunders; 2014. http://www.clinicalkey.com. Accessed June 11, 2014.
[9] Gonzalez F. Inflammation in polycystic ovary syndrome: Underpinning of insulin resistance and ovarian dysfunction. Steroids. 2012;77:300.
[10] Golden AK. Decision Support System. Mayo Clinic, Rochester, Minn.
April 25, 2014.
[11] Coddington CC (expert opinion). Mayo Clinic, Rochester, Minn. July
6, 2014.
[12] Knochenhauer ES, Key TJ, Kahsar-Miller M, Waggoner W, Boots LR, Azziz R. Prevalence of the polycystic ovary syndrome in unselected black and white women of the southeastern United States: a prospective study. J Clin Endocrinol Metab. 1998;83:3078–3082.
[13] Farah L, Lazenby AJ, Boots LR, Azziz R. Prevalence of polycystic
ovary syndrome in women seeking treatment from community electrologists. Alabama Professional Electrology Association Study Group. J Reprod Med. 1999;44:870–874. [PubMed]
[14] Stein IF, Leventhal ML. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstet Gynecol.1935;29:181–191.
[15] Rebar R, Judd HL, Yen SS, Rakoff J, Vandenberg G, Naftolin F.
Characterization of the inappropriate gonadotropin secretion in polycystic ovary syndrome. J Clin Invest. 1976;57:1320–1329.
[16] Azziz R, Dewailly D, Owerbach D. Clinical review 56: Nonclassic adrenal hyperplasia: current concepts. J Clin Endocrinol Metab. 1994;78:810–815. [PubMed]
[17] Silfen ME, Manibo AM, McMahon DJ, Levine LS, Murphy AR,
Oberfield SE. Comparison of simple measures of insulin sensitivity in young girls with premature adrenarche: the fasting glucose to insulin ratio may be a simple and useful measure. J Clin Endocrinol Metab. 2001;86:2863–2868. [PubMed]
[18] Legro RS, Finegood D, Dunaif A. A fasting glucose to insulin ratio is a useful measure of insulin sensitivity in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1998;83:2694–
2698. [PubMed]
[19] Ducluzeau PH, Cousin P, Malvoisin E, Bornet H, Vidal H, Laville M, Pugeat M. Glucose-to-insulin ratio rather than sex hormone-binding globulin and adiponectin levels is the best predictor of insulin resistance in nonobese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2003;88:3626–3631. [PubMed]
[20] Carnevale Schianca GP, Rossi A, Sainaghi PP, Maduli E, Bartoli E.
The significance of impaired fasting glucose versus impaired glucose tolerance: importance of insulin secretion and resistance. Diabetes Care.2003;26:1333–1337. [PubMed]
[21] Rosner W. An extraordinarily inaccurate assay for free testosterone is still with us. J Clin Endocrinol Metab.2001;86:2903. [PubMed]
[22] Derksen J, Nagesser SK, Meinders AE, Haak HR, van de Velde CJ.
Identification of virilizing adrenal tumors in hirsute women. N Engl J Med. 1994;331:968–973. [PubMed]
[23] Luciano AA, Chapler FK, Sherman BM. Hyperprolactinemia in polycystic ovary syndrome. Fertil Steril.1984;41:719–725. [PubMed]
[24] Franks S. Polycystic ovary syndrome: a changing perspective. Clin
Endocrinol (Oxf) 1989; 31:87–120.[PubMed]
[25] Pennsylvania State University College of Medicine, Hershey 17033, USA
[26] Bulun SE, Adashi EY. The physiology and pathology of the female reporductive axis. In: Kronenberg HM, Melmed S, Polonsky KS, Larsen PR, eds. Williams Textbook of Endocrinology. 12th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 17.
[27] Radosh L. Drug treatments for polycystic ovary syndrome. Am Fam
Physician. 2009; 79:671-676.
[28] Lobo RA. Hyperandrogenism: Physiology, etiology, differential diagnosis, management. In: Lentz GM, Lobo RA, Gershenson DM, Katz VL, eds. Comprehensive Gynecology. 6th ed. Philadelphia, Pa: Mosby Elsevier; 2012:chap 40.
[29] Sam S, Dunaif A. Polycystic ovary syndrome: syndrome XX? Trends
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 12, December-2014 521
ISSN 2229-5518
Endocrinol Metab. 2003;14:365–370. [PubMed]
[30] Alvarez-Blasco F, Botella-Carretero JI, San Millan JL, Escobar- Morreale HF. Prevalence and characteristics of the polycystic ovary syndrome in overweight and obese women. Arch Intern Med.
2006;166:2081–2086. [PubMed]
[31] Homburg R, Armar NA, Eshel A, Adams J, Jacobs HS Influence of serum luteinising hormone concentrations on ovulation, conception, and early pregnancy loss in polycystic ovary syndrome. BMJ.
1988;297:1024–1026.[PubMed]
[32] Glueck CJ, Wang P, Fontaine RN, Sieve-Smith L, Tracy T, Moore SK.
Plasminogen activator inhibitor activity: An independent risk factor for the high miscarriage rate during pregnancy in women with polycystic ovary syndrome. Metabolism. 1999;48:1589–95. [PubMed]
[33] Jakubowicz DJ, Iuorno MJ, Jakubowicz S, Roberts KA, Nestler JE.
Effects of metformin on early pregnancy loss in the polycystic ovary syndrome. J Clin Endocrinol Metab. 2002;87:5249. [PubMed]
[34] Gray RH, Wu LY. Subfertility and risk of spontaneous abortion. Am J Public Health. 2000;90:1452–4. [PMC free article] [PubMed]
[35] Boklage CE. Survival probability of human conceptions from fertilization to term. Int J Fertil 1990;35(2):75, 79–80, 81–94
[36] Wilcox AJ, Weinberg CR, O'Connor JF, et al. Incidence of early loss of
pregnancy. N Engl J Med 1988;319(4):189–194
IJSER © 2014 http://www.ijser.org