International Journal of Scientific & Engineering Research, Volume 5, Issue 5, May-2014 97
ISSN 2229-5518
Comparison of microalbuminuria with
biochemical and hematological parameters as a marker for renal involvement in patients at high risk for Chronic Kidney Disease – A pilot study.
Riju Mathew, Vinitha R Pai, Vijayakumar T.
Abstract— Estimation of urine microalbumin is considered as a novel marker for the assessment of early decline in glomerular function compared to the existing biomarkers such us creatinine especially in patients at high risk of developing CKD. Forty One patients (20 diabetic, 12 hypertensive and 9 both diabetic and hypertensive) at high risk for CKD and 19 healthy age and sex matched controls were included in the present study. Conventional renal biomarkers (Urine Protein, Protein Creatinine ratio, Serum Creatinine, Uric acid and Blood Urea), urine microalbumin and a complete blood count were estimated in all the subjects. Creatinine based eGFR using MDRD formulae and CG formula and cystatin C based eGFR were calculated. Microalbuminuria was found to be significantly correlating with serum creatinine, urine protein and urine protein creatinine ratio. Evaluation of the four eGFR equations showed a significant correlation. Among the hematological parameters ESR and the Platelet Count were found to be correlating with microalbuminuria. The study showed that the microalbuminuria is a better marker for the detection of early onset of CKD in high risk population like type 2 diabetes and hypertension.
Index Terms—Chronic Kidney Disease (CKD), Creatinine, Cockcroft-Gault (CG), Cystatin C, Estimated Glomerular Filtration Rate (eGFR), Glomerular Filtration Rate(GFR), Microalbuminuria, Microalbumin, Microalbumin creatinine ratio, Modification of Diet in Renal Disease (MDRD), Cockcroft-Gault (CG).
1 INTRODUCTION
—————————— ——————————
rinary excretion of albumin and lower molecular weight proteins is enhanced by factors that increase glomerular filtration load, either by saturating tubular reabsorptive capacity or as a result of increased tubular volume and flow rate[1],[2]. Under normal physiological conditions approxi- mately 99% of the filtered albumin is reabsorbed in the proxi- mal tubule and only trace of albumin is excreted through urine[3]. In pathological conditions when glomerular capillary wall permeability and/or filtration rate increase, albumin and other macromolecules excretion in urine also increases[4]. De- tection of increased urinary albumin excretion is of particular importance in the study of incipient renal disease5. Pro- teinuria itself causes renal injury by causing mesangial and tubule-interstitial damage[6],[7]. Studies have shown pro- teinuria itself as a major determinant of progressive renal fail-
ure[8],[9].
The term “microalbuminuria” (MAU) describes a urinary al-
bumin excretion that is increased but not to the level of overt
proteinuria. MAU is considered to be a risk factor for not only
nephropathy and progressive renal insufficiency in type 2 dia-
betes and hypertension but all cause mortality of the general
population[10],[11],[12]. Primary prevention of nephropathy
in diabetes and hypertension is feasible if the factors that initi-
————————————————
• Riju Mathew is currently pursuing PhD degree program at Yenepoya
University, Mangalore, India. E-Mail: rijumathewmsc@gmail.com
• Dr Vinitha R Pai is currently, Professor & Research guide, Dept of Bio-
chemistry at Yenepoya University, Mangalore, India.
• Dr Vijayakumar T is Professor, Research guide & Chief of Basic Medical
Sciences at Educare Institute of dental Sciences, Malappuram, India.
ate the change from normal urinary albumin excretion to MAU and from MAU to Nephropathy can be identified and treated[13],[14]. The determinants of microalbuminuria in- clude Blood pressure, Duration of diabetes[15], age[16], genet- ic factors[17], glycemic status and other micro and macro vas- cular diseases. Hematological parameters were reported to be useful in predicting renal involvement in hypertension[18].
The established classification of abnormal urine albumin ex- cretion according to the American Diabetic Association (ADA)[10] is given in Table 1.
Table 1. American Diabetic Association10 classification of abnormal UAE |
Category | Spot Urine collection (μg/mg creatinine) | 24-h Urine collection (mg/24 h) | Timed Urine collection (μg/min) |
Normal | < 30 | < 30 | < 20 |
Microalbuminuria | 30–299 | 30–299 | 20–199 |
Clinical albuminu- ria | ≥ 300 | ≥ 300 | ≥ 200 |
UAE: Urinary Albumin Excretion
Conventional markers like creatinine and urea have been used for years for the diagnosis and management of nephropathy in diabetes and hypertension. Cystatin C and creatinine based eGFR were reported to be useful in predicting renal involve- ment in high risk population. In the present study an attempt is being made to evaluate the efficacy of urinary microalbumin estimation as a better index for renal involvement in the high
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 5, May-2014 98
ISSN 2229-5518
risk population.
2 MATERIALS AND METHODS
The study is conducted in 60 subjects (41 patients and 19 Con- trols) after getting informed consent. In the patient group 20 were diabetic 12 were hypertensive and remaining where both diabetic and hypertensive. All the patients were on treatment for a period of five years and were well controlled. Patients with possible causes of proteinuria other than by CKD were excluded. All the investigations were performed at Medivision Scan and Diagnostic Research Centre Pvt Ltd., Cochin. Study questionnaire and Proforma were filled for each patient in- cluding ID, name, age, sex, present complaints, past history, family history of illness. The BMI and blood pressures of all the patients were recorded and urine samples and 5ml of fast- ing venous blood were collected. The complete blood cell count was analysed using Sysmex KX-21 analyser. Blood urea, creatinine, uric acid, CRP and urine microalbumin were esti- mated in Beckman AU 480 analyser. 2 mL of blood sample was collected from all the subjects 2 hours after food for PPBS. Quality controls were monitored using Bio-Rad quality control material. The eGFR were calculated using CG formula and MDRD and Abbreviated MDRD formulae[19]
The results were presented as mean ± standard devia- tion. The correlations between microalbumin and other pa- rameters were done using Pearson’s correlation analysis. P <
0.05 was defined as the limit of statistical significance. All sta- tistical analyses were performed using SPSS software version
17.0 and Minitab 16.0.
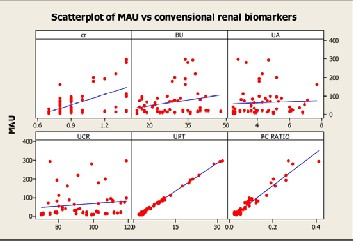
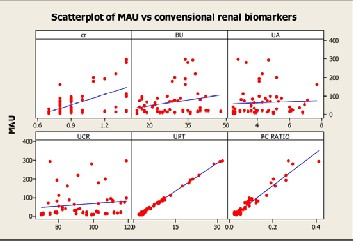
Figure 1: Scatter plot of Microalbuminuria against Conven- tional renal markers.
Key: Cr: Creatinine (mg/dL), BU: Blood Urea(mg/dL), UA: Uric acid(mg/dL), UCR: Urine Creatinine (mg/dL), UPT: Urine Protein (mg/dL), PC Ratio : Urine Protein Creatinine ratio.
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 5, May-2014 99
ISSN 2229-5518
3 RESULTS
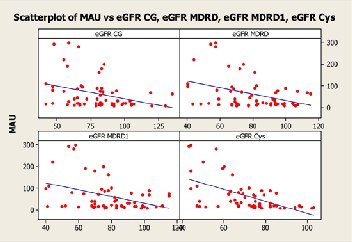
A comparative evaluation of microalbuminuria and conven- tional renal markers like creatinine urea and uric acid was carried out. Microalbuminuria was significantly correlating with urine protein, PC Ratio and Creatinine. There was no significant correlation between microalbuminuria and urea and uric acid (Table 3 and Figure 1). Correlation of microal- buminuria with estimated Glomerular Function tests eGFR is shown in Table 4 and Figure 2. There was a significant correla- tion of microalbuminuria with all eGFR equations under con- sideration. Cystatin C based eGFR was found to be a better index(r=-0.577) among the eGFR equations.
The physical and anthropometric data of the study population are summarized in Table 2. The systolic and dias- tolic blood pressure, BMI, fasting and post prandial blood sugar glycated hemoglobin and mean blood glucose of the test subjects were studied and compared with the controls. All the above values were found to be elevated in the test subjects compared to the normal controls.
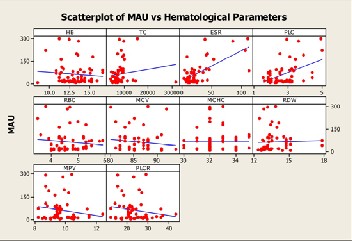
Correlation of microalbuminuria with RBC indices is shown in table 5 and Figure 3. There was no significant corre- lation between the microalbuminuria and the hematological parameters except for ESR and platelet count.
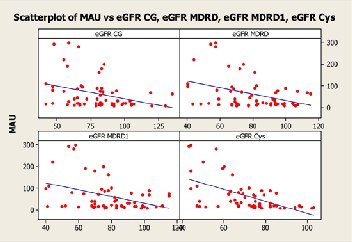
Figure 2 : Scatter plot of Microalbuminuria against estimat- ed Glomerular Filtration rate based on creatinine and cysta- tin C.
Key: eGFR : Estimated Glomerular Filtration rate, CG: Cockcroft-Gault, MDRD : Modification of diet in renal dis- ease, Cys: CystatinC
4 DISCUSSION
Diabetes and hypertension are the most common diseases which adversely affect the renal function[8],[20]. Early detec- tion of renal injury will help in the better management and prevention of progression of CKD to ESRD[21]. Many markers are being employed worldwide to detect renal involvement in these conditions[22].
Creatinine and CystatinC based eGFR are extensively employed as markers of renal injury[23]. It was shown earlier
that the MDRD and CG formulae were better creatinine based eGFR equations for the assessment of renal involvement in high risk population[24],[ 25]. The former lacks sensitivity and specificity and the latter is not cost effective. It was also re- ported that there is uncertainty in eGFR reported based on creatinine and cystatin C26 Hence in the study we have tried to evaluate the efficacy of urine microalbumin as predictive marker for renal involvement in the high risk population.
Table 5. Correlation of Microalbuminuria with hematologi- cal parameters |
N=60 | Pearson Correla- tion coefficient (r) | P value |
Hb(g/dL) |
TLC(Cells/Cumm) | 0.134 | 0.307 |
ESR (mm/hr) | 0.676 | <0.001 |
PLC (Lakhs/cumm) | 0.458 | <0.001 |
PCV(%) | -0.132 | 0.315 |
RBC (millions/cumm) | -0.115 | 0.380 |
MCV(fL) | -0.125 | 0.340 |
MCH (Pg) | -0.114 | 0.387 |
MCHC (%) | 0.000 | 1.000 |
RDW (%) | 0.024 | 0.854 |
PDW (fL) | -0.131 | 0.318 |
MPV (fL) | -0.184 | 0.159 |
Key: Hb: Hemoglobin, TLC: Total Leukocyte Count, ESR: Erythrocyte Sedimentation Rate, PLC: Platelet Count, PCV: Packed Cell Volume, RBC: red blood cells count, MCV: Mean Corpuscular Volume, MCH: Mean Corpuscular He- moglobin MCHC: Mean Corpuscular Hemoglobin concen- tration, RDW: Red cell distribution Width, PDW: platelet distribution width MPV: mean platelet volume |
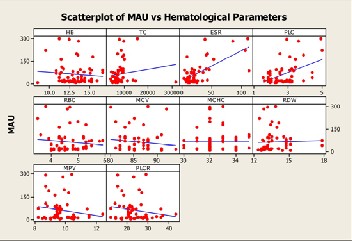
Figure 3 : Scatter plot of Microalbuminuria against hemato- logical parameters.
Key: HB: Hemoglobin, TC: Total Leukocyte Count,
ESR: Erythrocyte Sedimentation Rate, PLC: Platelet Count,
RBC: red blood cells count, MCV: Mean Corpuscular Vol-
IJSER © 2014 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 5, Issue 5, May-2014 100
ISSN 2229-5518

ume, MCHC: Mean Corpuscular Hemoglobin concentration,
RDW: Red cell distribution Width, PDW: platelet distribu- tion width, MPV: mean platelet volume
In the present study MAU is found be a better marker for predicting the progression of CKD which is well in agree- ment with the earlier studies by Powrie et al[13]. More over ESR which is reported to be a general health marker for all- time morbidity and mortality[27] is found to be correlating well with MAU. The non invasive nature and cost effective- ness makes urine microalbumin a better indicator for renal involvement in high risk population. This study clearly indi- cates the importance screening urine for microalbumin in all subjects with hypertension and type 2 diabetes Mellitus.
5 REFERENCES

[1] Haraldsson, Börje, Jenny Nyström, and William M. Deen. "Properties of the glomerular barrier and mechanisms of proteinuria." Physiolog- ical reviews 88, no. 2 (2008): 451-487.
[2] Metcalfe, Wendy. "How does early chronic kidney disease progress?
A background paper prepared for the UK Consensus Conference on early chronic kidney disease." Nephrology Dialysis Transplantation
22, no. suppl 9 (2007): ix26-ix30..
[3] Mogensen, CE. "Microalbuminuria predicts clinical proteinuria and early mortality in maturity-onset diabetes." New England journal of medicine 310, no. 6 (1984): 356-360.
[4] Mogensen, CE., and CK. Christensen. "Predicting diabetic nephropa- thy in insulin-dependent patients." New England Journal of Medi- cine 311, no. 2 (1984): 89-93.
[5] Mogensen, CE. "Microalbuminuria as a predictor of clinical diabetic nephropathy." Kidney int 31, no. 2 (1987): 673-689.
[6] D'amico, Giuseppe, and Claudio Bazzi. "Pathophysiology of pro- teinuria." Kidney international 63, no. 3 (2003): 809-825.
[7] Eddy, Allison A. "Proteinuria and interstitial injury." Nephrology
Dialysis Transplantation 19, no. 2 (2004): 277-281.
[8] Keane, William F., Barry M. Brenner, Dick De Zeeuw, Jean-Pierre Grunfeld, Janet Mcgill, William E. Mitch, Artur B. Ribeiro. "The risk of developing end-stage renal disease in patients with type 2 diabetes and nephropathy: the RENAAL study." Kidney international 63, no.
4 (2003): 1499-1507.
[9] Bernard, Alfred, and Robert Lauwerys. "Epidemiological application of early markers of nephrotoxicity." Toxicology letters 46, no. 1 (1989): 293-306.
[10] American Diabetes Association: Diabetic nephropathy (Position
Statement). Diabetes Care 2000; 23 (Suppl. 1):S69 –S72.
[11] Wang, Thomas J., Jane C. Evans, James B. Meigs, Nader Rifai, Caro- line S. Fox, Ralph B. D’Agostino, Daniel Levy, and Ramachandran S. Vasan. "Low-grade albuminuria and the risks of hypertension and blood pressure progression." Circulation 111, no. 11 (2005): 1370-
1376.
[12] Romundstad, Solfrid, Jostein Holmen, Kurt Kvenild, Hans Hallan, and Hanne Ellekjær. "Microalbuminuria and all-cause mortality in
2,089 apparently healthy individuals: a 4.4-year follow-up study. The Nord-Trøndelag Health Study (HUNT), Norway." American journal of kidney diseases 42, no. 3 (2003): 466-473.
[13] Powrie, J. K., G. F. Watts, J. N. Ingham, N. A. Taub, P. J. Talmud, and
K. M. Shaw. "Role of glycaemic control in development of microal-
buminuria in patients with insulin dependent diabetes." Bmj 309, no.
6969 (1994): 1608-1612.
[14] Zucchelli, Pietro, and Alessandro Zuccalà. "Hypertension and renal dysfunction." Current opinion in nephrology and hypertension 5, no.
1 (1996): 97-101.
[15] Basi, Seema, Pierre Fesler, Albert Mimran, and Julia B. Lewis. "Mi- croalbuminuria in Type 2 Diabetes and Hypertension A marker, treatment target, or innocent bystander?." Diabetes Care 31, no. Sup- plement 2 (2008): S194-S201.
[16] Chowta, N. K., P. Pant, and M. N. Chowta. "Microalbuminuria in diabetes mellitus: Association with age, sex, weight, and creatinine clearance." Indian journal of nephrology 19, no. 2 (2009): 53.
[17] Pinheiro, Sérgio VB, Anderson J. Ferreira, Gregory T. Kitten, Kátia D. da Silveira, Deivid A. da Silva, Sérgio HS Santos, Elisandra Gava et al. "Genetic deletion of the angiotensin-(1–7) receptor Mas leads to glomerular hyperfiltration and microalbuminuria." Kidney interna- tional 75, no. 11 (2009): 1184-1193.
[18] Jithesh, Tharayil Kattil, Riju Mathew, Vidyadharan Jayapal, and Thankappan Vijayakumar. "Microalbuminuria and Red Cell Distri- bution Width as Predictive Markers of Renal Involvement in Hyper- tension." International Journal of Health and Rehabilitation Sciences (IJHRS) 1, no. 2 (2012): 99-106.
[19] Launay-Vacher, Vincent, Hassane Izzedine, and Gilbert Deray. "Us- ing the right MDRD equation." Kidney international 66, no. 5 (2004):
2089-2089.
[20] Levey, Andrew S., Brad C. Astor, Lesley A. Stevens, and Josef Coresh. "Chronic kidney disease, diabetes, and hypertension: what's in a name&quest." Kidney international 78, no. 1 (2010): 19-22.
[21] Levin, Adeera, and Paul E. Stevens. "Early detection of CKD: the benefits, limitations and effects on prognosis." Nature Reviews Nephrology 7, no. 8 (2011): 446-457.
[22] Riju Mathew, Vinitha R Pai and Vijayakumar. T., “Comparative evaluation of conventional and new biomarkers of renal involvement in patients with type 2 diabetes mellitus and hypertension – a pilot study.” International Journal of Pharma & Bio Sciences 4, no. 2 (2013). 742 – 750.
[23] Ferguson, Michael A., and Sushrut S. Waikar. "Established and emerging markers of kidney function." Clinical chemistry 58, no. 4 (2012): 680-689.
[24] Jithesh, Tk; Riju Mathew; Jayapal., V; Vijayakumar, T. A comparison of eGFR using serum creatinine and cystatin for the assessment of renal involvement in hypertension. International Journal of Pharma
& Bio Sciences 4, no. 1 (2013) 1-9.
[25] Riju Mathew, Vinitha R. Pai, Ramesh K, Vijayakumar .T, Microalbu- minuria and estimated glomerular filtration rate (eGFR) using six prediction equations Proceedings in International conference on Pro- teomics and Genomics. (2011) p221-224.(Conference Proceedings)
[26] Badrie T., Turner P., “The Uncertainty of eGFR” Indian Journal of
Biochemistry 28 vol 3 (2013) 242-247.
[27] Stevens, D., R. Tallis, and S. Hollis. "Persistent grossly elevated eryth- rocyte sedimentation rate in elderly people: one year follow-up of morbidity and mortality." Gerontology 41, no. 4 (1995): 220-226.
IJSER © 2014 http://www.ijser.org