International Journal of Scientific & Engineering Research Volume 2, Issue 5, May-2011 1
ISSN 2229-5518
A Novel Real-time Intelligent Tele Cardiology
System Using Wireless Technology to Detect
Cardiac Abnormalities
S. Kohila, K. Gowri
Abstract - This study presents a novel wireless, ambulatory, real-time, and auto alarm intelligent telecardiology system to improve healthcare for cardiovascular disease, which is one of the most prevalent and costly health problems in the world. This system consists of a lightweight and power-saving wireless ECG device equipped with a built-in automatic warning expert system. A temperature sensor is fixed to the user’s body, which senses temperature in the body, and delivers it to the ECG device. This device is connected to a microcontroller and ubiquitous real-time display platform. The acquired ECG signals which are transmitted to the microcontroller is then, processed by the expert system in order to detect the abnormality. An alert signal is sent to the remote database server, which can be accessed by an Internet browser, once an abnormal ECG is detected. The current version of the expert system can identify five types of abnormal cardiac rhythms in real-time, including sinus tachycardia, sinus bradycardia, wide QRS complex, atrial fibrillation (AF), and cardiac asystole, which is very important for both the subjects who are being monitored and the healthcare personnel tracking cardiac-rhythm disorders. The proposed system also activates an emergency medical alarm system when problems occur. W e believe that in the future a business-card-like ECG device, accompanied with a Personal Computer, can make universal cardiac protection service possible.
Keywords - Atrial fibrillation (AF), ECG, Temperature Sensor, Expert Systems, Personal Computer, W ireless.
—————————— • ——————————
changing society with an improved quality of life and medical
1 INTRODUCTION
1.1 General Introduction
ARDIO Vascular disease (CVD) is one of the most prevalent and serious health problems in the world. An Estimated 17.5 million people died from CVD in 2005, representing 30% of all deaths worldwide. Based on current trends, over 20 million people will die from CVD by 2015. In
2000, 56% of CVD deaths occurred before the age of 75. However, CVD is becoming more common in younger people, with most of the people affected now aged between 34 and 65 years [1]. In addition to the fatal cases, at least 20 million people experience nonfatal heart attacks and strokes every year; many requiring continuing costly medical care. Developed countries around the world continue to experience significant problems in providing healthcare services, which are as follows:
1) The increasing proportion of elderly, whose lifestyle changes are increasing the demand for chronic disease Healthcare services;
2) Demand for increased accessibility to hospitals and mobile healthcare services, as well as in-home care [2];
3) Financial constraints in efficiently improving personalized and quality-oriented healthcare though the current trend of centralizing specialized clinics can certainly reduce clinical costs, decentralized healthcare allow the alternatives of in- hospital and out-hospital care, and even further, home healthcare [3]. Rapid developments in information and communication technologies have made it possible to overcome the challenges mentioned earlier and to provide a
services.
1.2 Sinus Tachycardia
Sinus tachycardia (also colloquially known as sinus tach or sinus tachy) is a heart rhythm with elevated rate of impulses originating from the sinoatrial node, defined as a rate greater than 100 beats/min in an average adult. The normal heart rate in the average adult ranges from 60–100 beats/min. Note that the normal heart rate varies with age, with infants having normal heart rate of 110–150 bpm to the elderly, who have slower normals. Tachycardia is often asymptomatic. If the heart rate is too high, cardiac output may fall due to the markedly reduced ventricular filling time. Rapid rates, though they may be compensating for ischemia elsewhere, increase myocardial oxygen demand and reduce coronary blood flow, thus precipitating an ischemia heart or valvular disease.
1.3 Sinus Bradycardia
Sinus bradycardia is a heart rhythm that originates from the sinus node and has a rate of under 60 beats per minute. The decreased heart rate can cause a decreased cardiac output resulting in symptoms such as lightheadedness, dizziness, hypotension, vertigo, and syncope. The slow heart rate may also lead to atrial, junctional, or ventricular ectopic rhythms. Sinus Bradycardia is not necessarily problematic. People who regularly practice sports may have sinus bradycardia, because their trained hearts can pump enough blood in each
IJSER © 2011 http://www.ijser.org
International Journal of Scientific & Engineering Research Volume 2, Issue 5, May-2011 2
ISSN 2229-5518
contraction to allow a low resting heart rate. Sinus Bradycardia can aid in the sport of Free diving, which includes any of various aquatic activities that share the practice of breath-hold underwater diving, Bradycardia aids in this process due to drop in blood rate pulse. These adaptations enable the human body to endure depth and lack of oxygen far beyond what would be possible without the mammalian diving reflex. Sinus bradycardia is a sinus rhythm of less than 60 bpm. It is a common condition found in both healthy individuals and those who are considered well conditioned athletes. Studies have found that 50 - 85 percent of conditioned athletes have benign sinus bradycardia, as compared to 23 percent of the general population studied. Trained athletes or young healthy individuals may also have a slow resting heart rate.
1.4 Wide QRS Complex
A widened QRS ("'120 msec) occurs when ventricular activation is abnormally slow, either because the arrhythmia originates outside of the normal conduction system (e.g., ventricular tachycardia), or because of abnormalities within the His-Purkinje system (e.g., supraventricular tachycardia with aberrancy).
1.5 Atrial Fibrillation
Atrial fibrillation (AF) is the most common cardiac arrhythmia, affecting nearly 1% of the population. Its prevalence increases with age; although relatively infrequent in those under 40 years old, it occurs in up to 5% of those over 80. Most people with a normal sinus rhythm have a resting heart rate of between 60 and 100 beats per minute. In AF patients, the atria contract rapidly and irregularly at rates between 400 to 800 beat per minute. Fortunately, the atrioventricular node compensates for this activity; only about one or two out of three atrial beats pass to the ventricles [4]. A typical ECG in AF shows a rapid irregular tachycardia in which recognizable P waves are sometimes absent. The ventricular rate in patients with untreated AF is generally 110 to 180 beats per minute. However, slower ventricular rates may occur in elderly patients with untreated AF. Data from the Framingham study demonstrates that chronic heart failure is associated with a 4.5- fold increase in risk of AF in men and a 5.9-fold increase in women. Apart from the epidemiological data, most evidence on the prevalence of AF in heart failure patients stems from analysis of a number of clinical trials conducted within the last
10–15 years on populations with heart failure. AF might have no detectable CVD. Hemodynamic impairment and thromboembolic events related to AF patients included in these trials were selected for different purposes, which are reflected in the varying prevalence of AF. In addition, AF often associated with structural heart disease, causes significant morbidity, mortality, and healthcare cost in a substantial proportion of patients, thus making it a major global healthcare challenge. In this study, we attempted to develop an intelligent expert system with a built-in abnormal ECG-detection mechanism in the telecardiology healthcare service to facilitate
diagnosis and management of patients with AF and other rhythm disorders [6]. Simplicity, reliability, and universality are the main concepts behind this service. Therefore, this study constructs a ubiquitous and intelligent telecardiology healthcare network consisting of a miniature wireless ECG device embedded with an alert expert system for the early detection of cardiac disorders.
1.6 Cardiac Asystole
Asystole is a state of no cardiac electrical activity; hence no contractions of the myocardium and no cardiac output or blood flow. Asystole is one of the conditions required for a medical practitioner to certify death. While the heart is asystolic, there is no blood flow to the brain unless CPR or internal cardiac massage is performed, and even then it is a small amount. After many emergency treatments have been applied but the heart is still unresponsive, it is time to consider pronouncing the patient dead. Even in the rare case that a rhythm reappears, if asystole has persisted for fifteen minutes or more the brain will have been deprived of oxygen long enough to cause brain death.
2 OVERALL SYSTEM
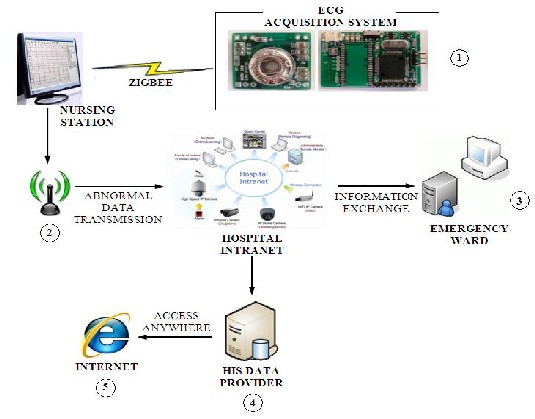
The system proposed in this study uses a Three-lead wireless ECG device, a microcontroller expert system, and a Web-based monitoring platform to meet these objectives. A small, three- lead ECG device is first set up using electrodes, affixed to areas on the user’s body. A temperature sensor is fixed to the users body, which senses temperature in the body and deliver it to the ECG device. This lightweight ECG can be connected to portable devices, such as a notebook or mobile phone, using ZigBee Module. The programming application installed on a microcontroller in ECG Device can then initiate data recording and data transmission. Successive data are transmitted to a portable device and processed in a period of 6 s by an expert system. The lead signal, coordinated with the direction of cardiac conduction pathway is extracted for signal analysis. As long as an abnormal ECG signal was detected, the system automatically transmitted data over a Wi-Fi/3G/2G networks to a remote data server (see Fig 1). At the same time, the system will send out an alert message to a nursing station in the cardiovascular ward for further examination. If necessary, the emergency ward or other departments can also access this data through an intranet. With the convenience of the world-wide Web protocol, anyone, including physicians, nurses, and family members, can access the data server and monitor real- time ECG plots using a Web browser, such as Internet Explorer (IE). For patients admitted to a cardiovascular ward or intensive care unit (ICU), the proposed cardio-healthcare system provides greater freedom of movement than products currently on the market [7]. Paring lightweight wireless ECG devices with mobile phones offers continuous and reliable patient monitoring. A warning system is also activated when unstable ECGs appear.
IJSER © 2011 http://www.ijser.org
International Journal of Scientific & Engineering Research Volume 2, Issue 5, May-2011 3
ISSN 2229-5518
Whenever the person moves his body temperature rises due the work done, and the degree of increase is based on the amount of work done. Also if a person got any fever his heart beat may increase which may be misrecognized as an
abnormal heart condition on an average the heart beat increase
for an average of 7-8beats for every single degree increase in temperature. Here in the proposed work the constraint has been considered and the problem has been faced better. In the proposed system Zigbee module is used, which is fully secured
and provide full duplex transmission. This will enhance the
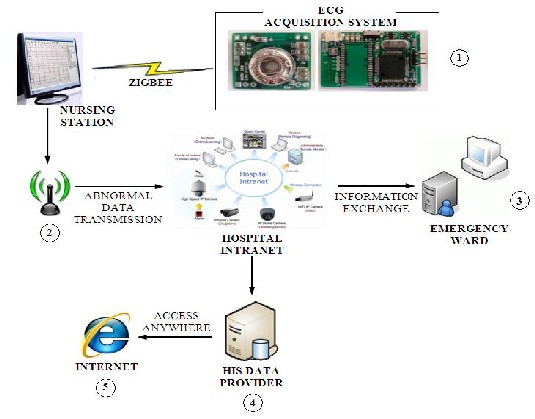
Fig 1: Flowchart of proposed system.The System uses a 5 lead ECG acquisition device ,the Abnormality detection Algorithm in the device detect the abnormal ECG signal and a W eb-based monitoring window allowing access to the data server and plot in real time by using an IE browser. Step()): The Signal are acquired by the ECG Electrodes Step@: The Abnormality in signal is detected and transferred to the hospital intranet, StepCi:The information from intranet is moved to the emergency ward database, Step®: The information from the intranet is also moved to the hospital intranet server, Step@: The abnormality information can be accessed by anyone through web service.
way of wireless communication used in the system. ZigBee targets the application domain of low power, low duty cycle and low data rate requirement devices.
3 ECG DEVICE WITH WIRELESS UNIT
The Hardware Circuit Designed Using all the Required parts (5 ECG electrode, Pre Amplifier, Band Pass Filter, Amplifier, PIC Microcontroller, ADC, Zigbee Module) [8]. The proposed three-lead ECG device contains two main parts: The Analog unit and The Digital unit (see Fig 2).
3.1 Analog Unit
The DAQ unit integrates an analog preamplifier, filter, and an AD converter (ADC) into a small (20 × 18 mm2), lightweight, and battery-powered DAQ system. The ECG signal is sampled at 512 Hz with 12-bit resolution, amplified by 100 times, and band pass filtered between
1 to 150 Hz. To reduce the number of wires for high- density recordings, the
IJSER © 2011 http://www.ijser.org
International Journal of Scientific & Engineering Research Volume 2, Issue 5, May-2011
4
ISSN 2229-5518
Fig 2: Block Diagram of ECG Device
power clocks, and measured signals are daisy-chained from one node to another with bit-serial output. Therefore, adjacent nodes (electrodes) are connected together to 1) share the power, reference voltage, and ADC clocks and 2) daisy chain the digital signal outputs.
3.2 Digital Unit
The Digital unit consists of a wireless module and a microcontroller. This unit uses a Zigbee module to send the acquired ECG signals to a Zigbee Enabled PC, serving as a real-time signal processing unit. All modules included one wireless-transmission unit and three DAQs, the theoretical maximum running time is estimated at about 33 h when using an 1100 mA·h Li- ion battery with continuous acquisition and transmission of the physiological signal to the expert system[9].
4 QRS WAVE DETECTION ALGORITHM
The ECG signals are amplified and recorded with a sampling rate of 512 Hz and band pass filtered between
1 and 150 Hz. Artifacts were removed before R peak detection. A 50 Hz notch filter is used to eliminate the power line interference, producing high-frequency, noise-free, and smooth data. Two segments of the baseline signal are extracted to compute mean and standard deviation (SD). Besides, the QRS detector requires the first and second-order derivative of the preprocessed ECG signal.
The latter gives spikes at the fiducial points. There are also false spikes, but their relative magnitudes are lower than those of the spikes at the
fiducial points. Accordingly, the R peak is clipped by higher magnitude negative peaks and high positive peaks in the first derivative plot. The procedure of defining the QRS complex onset is as follows: after 256 ms of flat segment in the ECG, the first sample, where the slope becomes steeper (high positive peaks) than the higher slope threshold, is defined as the QRS onset. The lower slope threshold is used to detect the higher magnitude negative peaks. Both thresholds are updated to search for missing beats. After identifying the QRS onset, the R peak is labeled by searching for the maximal value of the ECG samples in the 36 ms following the QRS onset. When R peak is determined, the QRS detector searches forward and backward to identify the two most negative points on the ECG plot and labels them as the Q wave peak and the S wave peak, respectively. The black curve means the normal ECG signal which contains three waves. The dotted line shows the first deviation of the normal ECG signal (see Fig 3). Results show that full squares wave peak
.
Fig 3: QRS detection in the normal ECG waves .
mark the R wave peaks, full circles mark the Q s, and full star mark the S wave peak. QRS onset is defined by the vertical line.The QRS complex duration is set from QRS onset time to 20 ms after the S wave peak
5 ABNORMAL ECG DETECTION
After defining the QRS complex and the Q, R, and S wave peak, we then sought to detect common and important rhythm disorders, including sinus tachycardia, sinus bradycardia, cardiac systole, AF, and wide QRS complex. Sinus tachycardia is detected by the condition of the heart rate >100 beats per minute. An asystole indicates the situation of no heart rate.
IJSER © 2011 http://www.ijser.org
International Journal of Scientific & Engineering Research Volume 2, Issue 5, May-2011
5
ISSN 2229-5518
Wide QRS complex occurred as the duration of QRS complex was greater than or equal to 120 ms. C. AF Detection Since an irregular rhythm of the QRS complexes is the major feature of AF, the R–R interval (RRI), defined as the interval of neighboring QRS complexes, is an ideal parameter to identify AF. This study uses two different algorithms for AF detection.
5.1 Algorithm I for Abnormal ECG Detection: Step 1: Detection of R waves and marking of R peaks. Step 2: Calculation of RRI (the duration of adjoined R
peaks).
Step 3: Calculation of the variation of consecutive RRI
(L1RRI).
Step 4: Activation of the alarm system when L1RRI>150
ms occurs twice within each 6 s of computation.
5.2 Algorithm II for Abnormal ECG Detection Step1: Detection of R waves and marking of R peaks. Step2: Calculation of RRI (the duration of adjoined R
peaks).
Step3: Counting the number of peaks to calculate the number of beats in each 6s.
Step4: Check whether temperature ranges between 33-
370 continue the process, else go to Step 8
Step5: Calculation of the variation of consecutive
RRI(L1RRI).
Step6: Calculation of the SD of RRI (RRIstd) in each 6-s
recording.
Step7: Activation of the alarm system when L1RRI>150 ms occurs twice and RRIstd > 60 ms within 6 s of computation.
Step8: Measuring the heartbeat, up to 180bpm is considerable during very high fever.
Theoretically, Algorithm I is more accurate in detecting an irregular ventricular rhythm, though in detecting frequent pre mature beats during uncommon, it is difficult to differentiate the Atrial Fibrillation from Premature Beats. To overcome this problem, we formulated Algorithm II, which uses a cut-off value of RRIstd>60 ms for AF detection. This condition shows that whenever the standard Deviation of RRI exceeds
60ms the system will produce an alert signal. The cut- off value of 60 ms was based on comparing 50 normal subjects’ and 50 patients having cardiac abnormality’ Also Algorithm II will produce an accurate detection considering the temperature of the patient Fig. 4 shows statistical results of the differences between normal and AF patients regarding L1RRI and RRIstd. Accordingly,
the threshold level of L1RRI and RRIstd were given as
150 and 60 ms, respectively.
6 RESULTS AND DISCUSSIONS
In order to analyze the performance of the abnormality detection algorithm, the device is fixed to 10 patients who underwent treatment at General Hospital.Analysis and Performance Calculation was performed according to the recommendations of the American National Standard for ambulatory ECG analyzers (ANSI/AAMI EC38–1994) [11]. A true positive (TP) shows that the algorithm successfully detected abnormality for abnormal subject during every 6 s of computation. On the other hand, a false negative (FN) shows a failed detection of abnormality for an abnormal patient. Finally, false positive (FP) represents a false detection of abnormality, whereas true negative (TN) means normal subjects have no abnormality detection. Accuracy, sensitivity and positive predictive values were used for further analysis. The recorded data were shown in Tables 1 and 2 for normal and abnormal patients under testing for different algorithms. The subjects tested for abnormalities were of age group greater than 50. Table 1 shows the abnormality detection in subjects using Algorithm I.
TABLE 1
Abnormality Detection in Subjects Using Algorithm I
Subject/ Condition (N=10) | Positive Test | Negative Test | Total |
Abnormal patients | 187 | 8 | 195 |
Normal patients | 5 | 0 | 5 |
Total no. of tests | 200 |
TABLE 2
Abnormality Detection in Subjects Using Algorithm II
IJSER © 2011 http://www.ijser.org
International Journal of Scientific & Engineering Research Volume 2, Issue 5, May-2011
6
ISSN 2229-5518
Total no. of tests 200
Fig 5: Analysis of Average Performance between two Algorithms.
Totally 10 subjects were tested and each were tested 20 times, hence there will be totally 200 tests undergone. Each test was recorded for duration of 6 sec. Hence the total duration for each subject will be 2 min. This algorithm shows 100% for normal subjects and with little difference in case of abnormal subjects. Similarly, Table 2 shows the abnormality detection in subjects using Algorithm II. While considering Algorithm I the average accuracy was 93.5%, its sensitivity performance is 95.9%, and the positive predictive value is 97.4% (see Fig 5). The same 10 patients were also tested using Algorithm II, in which abnormality is detected only when three conditions were met. i.e.,
(i) L1RRI>150 ms occurs twice
(ii) RRIstd > 60 ms within 6 s of computation and
(iii) Considering body temperature.
The average accuracy, sensitivity, and positive predictive performance were 96%, 97.5%, and 98.5% (see Fig 5) respectively. Comparing the performance of both Algorithms I and II, the performance in Algorithm II was much better. These results showed that combining the three conditions as the detection criteria in Algorithm II, will improve the abnormality detection performance, especially in terms of accuracy and sensitivity performance. Among a total of 10 patients, Algorithm II displays the stable and high impact results across subjects. The results suggest that our system can provide a reliable abnormality detection function in telecardiology healthcare services.
7 CONCLUSION
AF, the most common sustained cardiac arrhythmia, causes significant mortality and morbidity, and remains a major healthcare challenge [11]. Early detection is very important for providing appropriate therapeutic interventions and managing disease related complications, such as congestive heart failure and stroke. This study demonstrates that the proposed intelligent telecardiology system is capable of accurately detecting AF episodes and instantaneously alerting both the user and the healthcare personnel, facilitating early medical intervention. Furthermore, this intelligent telecardiology system is superior to conventional healthcare devices because it integrates all the key elements in one system. The following list describes the most important features of the proposed system
1) Wireless: Communications between devices are all
wireless (Zigbee), reducing wire stock usage and
allowing convenient operation.
2) Ambulatory: The miniature ECG device is very lightweight, can easily be applied to the body, and can operate for a considerable length of time. The system can be run anywhere with a notebook or mobile phone, eliminating the problems of limited power or restricted areas.
3) Real time: ECG signals can be transmitted to nearby mobile devices instantly and there is only a few seconds lag when the signals are transmitted to a remote database server, depending on network capacity.
4) Self-alarm: The built-in expert system automatically detects abnormal ECG signals and alerts both the user
and healthcare personnel using a Internet, or by sending a message to a remote database server installed in the hospital computer system and the emergency service system.
This novel system cannot only be used for inpatients and outpatients, but also provides a long- lasting health monitor to normal people. Patients wearing the lightweight three-limb lead wireless ECG device can hardly feel its presence, but still enjoy a sense of protection.
However, there are several limitations for the expert system. First, Abnormality detection is based on the RRI variation, when the user has frequent atrial or ventricular premature beats, which can be misdiagnosed as AF. Second, in patients with Cardiac Abnormality and markedly impaired AV nodal conduction, RRI variations may become too small for the system to diagnose Abnormality accurately. Lastly, there is still considerable motion noise during the recording, which might impair diagnostic accuracy. In conclusion, this novel intelligent telecardiology system
IJSER © 2011 http://www.ijser.org
International Journal of Scientific & Engineering Research Volume 2, Issue 5, May-2011
7
ISSN 2229-5518
is capable of early Abnormality detection, and represents a successful first step toward improving efficiency and quality of care in CVD. Further researches aimed at improving both hardware and software designs are necessary to enhance the efficiency and accuracy in future models of this system.
8 ACKNOWLEDGEMENT
The Authors would like to thank The Principal and Head of the Department of KSR College of Engineering for their constant support; also they thank Dr.T.Gayathri M.B.B.S for her great help in providing clinical guidance.
9 REFERENCES
[1]. World Health Organization, ‘The World Health Report
2008, ‘World Health Organization’, Geneva,2008.Available:http://www.who.int/whr/2008/whr08
_en.pdf
[2]. Koch.S,(2006) ‘Home telehealth—Current state and future trends,’ Int. J. Med. Inf., vol. 75, pp. 565–576.
[3]. Romanow, R.J. (2002, Nov.). ‘Building on values: The future of healthcare in Canada—Final report’. Commission of the Future of Health Care, Ottawa, Canada [Online]. Available: http://www.cbc.ca/he althcare/ final_report.pdf
[4]. Waktare.J.E.P, (2002) ‘Atrial fibrillation,’ Circulation, vol.
106, pp. 14–16.
[5]. Hurst. J, ‘Naming of the waves in the ECG, with a brief account of their Genesis’.
[6]. Kannel.W.B and McGee.D.L,(1979) ‘Diabetes and cardiovascular disease. The Framingham study,’ J. Amer. Med. Assoc., vol. 241, no. 19, pp. 2035– 2038.
[7]. Amer. Coll. Cardiol.J (2006) ‘ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation,’ vol.
48, pp. 149–246.
[8]. Vanagas.G, Zaliunas.R, Benetis.R, and Slapikas.R,(2008)
‘Factors affecting relevance of tele-ECG systems application to high risk for future ischemic heart disease events patients group,’ Telemed. J. e-Health, vol. 14, no. 4, pp. 345–349.
[9]. Lin.C.T, Ko.L.W, Chang.C.J, Wang.Y.T, Chung.C.H, Yang.F.S, Duann.J.R, Jung.T.P, and ChiouJ.C,(2009)
‘Wearable and wireless brain computer interface and its applications,’ presented at the 13th Int. Conf. Human Computer Interface, San Diego, CA.
[10]. Pang.L, Techoudovski.I, Braecklein.M, Egorouchkina.K, Kellermann.W and Bolz.A,(2005) ‘Real time ischemia detection in the smart home care system, ‘in Proc.
27th Annu. Conf. IEEE Eng. Med. Biol., Shanghai, China, Sep. 1–4, pp. 3703–370
[11]. American National Standard for Ambulatory
Electrocardiographs, ANSI/AAMI EC38–1994, 1994.
[12]. Papaloukas.C, Fotiadis.D.I, Likas.A, Stroumbis.C.S, and Michalis.L.K,(1998) ‘Use of a novel rule-based expert system in the detection of changes in the ST segment and the T wave
in long duration ECG,’ J. Electrocardiol., vol. 35, no. 1, pp.
27–34, 2002,” Circulation, vol. 98, pp. 1937–1942.
IJSER © 2011 http://www.ijser.org