

International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1498
ISSN 2229-5518
Dr. Aakanksha Rathor,PGT ENT ; Dr. Smrity Dutta , Asst. Prof., Deptt. Of
Otorhinolaryngology, Silchar Medical College And Hospital.
SUMMARY: 3 case reports of tuberculosis at uncommon sites within head and neck region. Diagnosed on the basis of various clinical, histopathological and imaging studies. Managed either with DOTS regimen only or both surgery & antitubercular treatment. None of the cases showed non-compliance to treatment or recurrence of disease.
KEYWORDS: tuberculosis, intra parotid lymphadenitis, branchial cyst, jugular chain lymphadenitis level
II-III.
INTRODUCTION:
As the medical science has advanced to its zenith, downward trend in pulmonary tuberculosis & its complications, with simultaneous upward trend of extrapulmonary tuberculosis has caused perpetuation of this disease [1].
India accounts for nearly 1/5th of the global tuberculosis [2]. A formidable challenge in its elimination. EPTB is more likely to occur with HIV co-infection. [3,4]
We report three cases of extra pulmonary tuberculosis .The unique feature which is highlighted is that tuberculosis is primary and is in immunocompetent patients with negative ELISA , blood counts within normal limits and no history of diabetes mellitus.
1. Intraparotid lymph node enlargement due to tuberculosis is a rare finding. The most likely differential diagnosis is a parotid tumor [Indian Journal of otolaryngology-Unilateral Tuberculosis of parotid gland].
The existence of a known parotid swelling with a unilateral firm , painless & an enlarged lymph node in posterior triangle of neck but no history of tuberculosis may suggest a neoplasm. The early diagnosis & treatment is important as the patient may undergo excision & may result in an inevitable fistula or facial nerve paralysis.Therefore,
FNAC, USG parotid region & Montaux test are important.
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1499
ISSN 2229-5518
Clinically it has been seen that the salivary gland involvement is secondary to systemic dissemination, which is a rare event. But in our case intraparotid lymphadenitis was a primary tuberculosis which in itself is rarest.
2. Branchial cyst tuberculosis is exceptionally rare & poorly described in the literature. It may be more common in patients with disseminated tuberculosis or immunocompromised states. However, it can be an isolated branchial cyst tuberculosis as was our case.
3. Lymph node tuberculosis has increased over years .It has become 2nd common to pulmonary tuberculosis [5]. Tuberculous cervical lymphadenitis is the most frequent manifestation of EPTB [6,7,8].This proportion of EPTB is almost 46.2 % much higher in lymph nodes. The classical presentation of tubercular lymphadenitis is unilateral, painless, firm, erythematous swelling in posterior triangle of neck.[9,10]
In our case the lymphadenitis was of jugular chain level II-III, huge in size & hard in consistency which pointed more towards malignancy rather than tuberculosis.
MATERIAL & METHODS :
CASE 1 :
A 35 years old female presented with a swelling over left pre-auricular region for the last 2 months from the date of examination. It was a size of a gram when first noticed by the patient on self palpation.
The swelling has enlarged uniformly over the time up to present size of about a walnut.
There is no history of pain or increase in size of swelling during meals or difficulty in opening mouth.
There is no associated pain, watery discharge from swelling or local rise of temperature.
There are no aggravating or relieving factors.
There is no history prolonged cough, chest pain, hemoptysis or evening rise of temperature.
Patient, till the date of starting treatment, had no difficulty in closing the eyes, drooling of saliva from the angle of mouth, any difficulty in opening mouth or collection of food
material in the vestibule of mouth.
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1500
ISSN 2229-5518
There is no history of dry eyes or dry mouth.
There is no history of sensation of blocked ear.
There is no loss of appetite, loss of weight; fatigue.The patient has a history of caries of left upper 1st molar.
The patient has no history suggestive of tuberculosis, diabetes mellitus or past hospital admissions or fever of unknown origin or septicemia or draining sinuses over the body.
The patient gives history of exposure with a person suffering of tuberculosis in neighbourhood.
ROUTINE BLOOD EXAMINATION: All parameters are within normal limit except Hb =
10.1 g/dl & ESR of 40 mm AEFH (WINTR) while ELISA was non-reactive.
USG OF PAROTID REGION:
Evidence of enlarged intra parotid lymph nodes are noted measuring 20mm x 10 mm x
10 mm.Multiple mildly enlarged lymph nodes 13 -14 mm are also noted along (L) jugular chain above carotid bifurcation.(L) Parotid gland parenchyma is normal in size & echo
pattern.
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1501
ISSN 2229-5518
A provisional diagnosis of infection or neoplasm was made & a FNAC was advised. On aspiration with a needle frank pus came out but no organisms were isolated from culture.
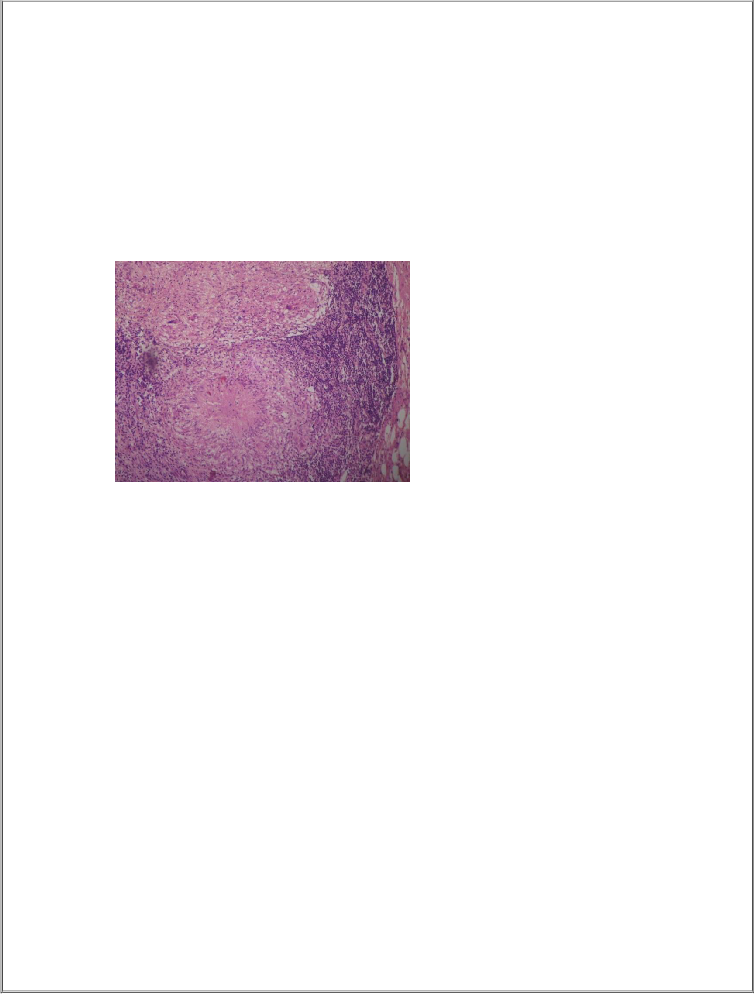
FNAC FROM PAROTID SWELLING: Cytology suggested granulomas made of epithelioid cells & occasional giant cells surrounding caseous necrosis.The FNAC opinion was granulomatous lymphadenitis
FNAC from cervical lymph node also suggested granulomatous lymphadenitis.
MONTAUX TEST revealed Erythema (+) & induration of 10mmx12mm, The skin test is almost always positive (> 10 mm induration) [11]
Skiagram of chest (PA view) was normal while the skiagram of ipsilateral upper
premolars & molar teeth showed periapical caries of 1st molar with caries & cavitation of
3rd molar tooth.
The antitubercular treatment was started as per RNTCP.patient is on regular follow up after 30
& 60 days and on examination there was reduction in size of both parotid gland swelling and cervical lymph node.
Repeat USG PAROTID REGION revealed evidence of enlarged parotid lymph nodes about the size of 10 mm x 7.2 mm. (L) parotid gland parenchyma is normal in echo texture. This shows
reduction in the size of intraparotid lymph nodes.
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1502
ISSN 2229-5518
CASE 2: An 18 year old girl from silchar, Assam presented with complaints of recurrent swelling on left side of neck for the last 2 years. This was associated with intermittent pain and
mucopurulent discharge from the region.
She had undergone incision and drainage of the neck abscess elsewhere at least 5 times within these 2 years. Clinical examination reveals a soft, fluctuant, tender, ovoid swelling approximately 7cmx 5cm in its greatest dimensions .Extending from anterior border of (L) sternocleidomastoid muscle to about 1 cm lateral to midline. Vertically it extended from the level of hyoid to the junction of middle & lower 1/3 of anterior border of (L) sternocleidomastoid muscle.
The USG of neck revealed it to be a ruptured branchial cyst.
Again an incision & drainage was done and about 60 ml of a foul smelling, mucopurulent fluid was aspirated. It was sent for culture & sensitivity which was reported to be organism klebsiella spp with sensitivity to ofloxacin/moxacillin/norfloxacin/imepenem & cefaperazone antibiotics.
Flexible laryngoscopy revealed no abnormality. Barium swallow showed normal study.
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1503
ISSN 2229-5518
Fistulogram revealed: collection noted at the level of (L) transverse process of C7 vertebra. Chest x-ray was normal.
Her Hb = 8.6g/dl ESR= 40 mm AEFH (WINTROBES); Lymphocyte count as 50.4 %.
After subsidence of active inflammatory state the cyst was opened. The walls of the cyst were quite friable & were sent for histopathological examination. Intra-operatively cyst extended about 2cm lateral to midline to anterior border of (L) sternocleidomastoid muscle .Above, from the level of hyoid to the junction of middle and lower 1/3 of the (L) sternocleidomastoid
muscle. The whole cyst was excised with no intra- operative complications.
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1504
ISSN 2229-5518
The biopsy report was suggestive of tuberculosis. The patient was put on ATT of DOTS strategy. Till the date patient has no recurrence and is doing well.
CASE 3: An 8years old boy hailing from silchar presented in our hospital with a diffuse,
hard swelling over the left sternocleidomastoid muscle for the last 6 months. There was gradual increase in size of the swelling with restriction of movement of neck. There was no history of prolonged cough, chest pain or fever.
On examination swelling extended from left angle of mandible over the stenocleidomastoid muscle up to the junction of middle 1/3rd & lower 1/3rd.It was about 7cm x 5cm in its greatest dimensions, hard in consistency, not adherent to overlying skin or fixed to underlying structures. The overlying skin appeared normal.
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1505
ISSN 2229-5518
USG neck suggested multiple conglomerated nodes with internal areas of necrosis noted in left cervical region.
FNAC FROM THE LYMPHNODES showed feature suggestive of granulomatous lymphadenitis, possibility of tubercular lymphadenitis be considered.
Routine blood examination revealed Hb = 9.1 g/dl, lymphocyte count =20.1 %, ESR= 30 AEFH (WINTROBE)
Chest x-ray was normal. Incision biopsy was taken during which foul smelling fluid was also aspirated & sent for culture & sensitivity. Tuberculosis was reported.
Patient is on ATT of DOTS strategy and doing well. The swelling has reduced in size &
consistency is now firm.
1. Tuberculosis, a chronic granulomatous disease, in parotid gland is an unusual & unique presentation because :
a. There is absence of any primary pulmonary foci
b. Without typical features of tuberculosis. c. Patient is immunocompetent.
The horns in the diagnostic dilemmas led us to resort to FNAC, USG of parotid region & histopathological examination. The source of the infection was probably from caries 1st upper molar tooth [12].
2. The diagnosis of branchial cyst requires a high index of suspicion because of vague clinical manifestations esp. in patients with recurrent neck abscesses that donor respond to
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1506
ISSN 2229-5518
appropriate medical therapy[13]. The treatment of branchial cyst with tuberculosis should be excision and DOTS therapy.
3. Details of investigations performed to diagnose tubercular lymphadenitis were FNAC; biopsy, direct smear and USG of neck are required. Literature suggests AFB is seen in 20 out of 77 in casseating & 1 in 20 non-casseating granuloma of tuberculosis [14].
The FNAC is diagnostic for tuberculosis showing specific granulomatous lesions with giant cells
& necrosis. [15]
Short course chemotherapy for tubercular lymphadenitis has shown encouraging results. [16]Hence, Tuberculosis diagnosis requires high degree of suspicion when the primary is at unusual sites. We could not find any specific symptoms that can be attributed to tuberculosis at these respective sites. In our case, these patients responded very well without any dissemination.
However outcome is also influenced by co-morbid illness and extent of the disease process.
Our study supports the fact, into its known existence; tuberculosis continues to contribute significantly to several other known & unknown diseases.
1. Sharma SK, Mohan A.Extrapulmonary Tuberculosis. Indian J Med Res 2004;120:316-53
2.V.K.Dhingra And Shadbad Khan. A Sociological Study On Stigma Among Tb Patients In Delhi. Indian J Tuberc 2010 ; 57: 12-18.
3.Shafer RW, Kim DS, Weiss JP,Quale JM.Exrapulmonary Tuberculosis In Patients With Human
Immunodeficiency Virus Infection. Medicine (Baltimore) 1991;70 :384-97
4.Steinbrook R. HIV In India-A Complex Epidemic. N Eng J Med 2007; 356 : 1089-93.
5.Kabra SK ,Lodha R,Seth V. Tuberculosis In Children What Has Changed In Last 20 Years? Indian J Pediatr.2002 Nov; 69 Suppl 1:S5-10. Indian Pediatr 2004 Sep; 41(9): 927-37.
6.Appling D, Miller RH: Mycobacterial Cervical Lymphadenopathy: 1981 Update.Layngoscope 1981;
91:1259
7.Castro DJ: Cervical Mycobacterial Lymphadenitis: Medical Vs Surgical Management. Arch Otolaryngol
1985; 111:816.And Others.
8.Dietel M: Treatment of Tuberculous Masses in the Neck. Can J Surg 1984; 27: 90 And Others.
IJSER © 2013
International Journal of Scientific & Engineering Research, Volume 4, Issue 4 , April-2013 1507
ISSN 2229-5518
9.Manolidis S: Mycobacterial Infections of the Head & Neck. Otolaryngol Head Neck Surgery 1993; 109:
427 and Others.
10.Lee Kc, Schecter G: Tuberculous Infections of the Head and Neck. Ear, Nose, Throat J 1995; 74:395
11.Howkins DB: Mycobacterial Cervical Adenitis in Children: Medical and Surgical Management. Ear, Nose, Throat J 1993; 72:733. And Others
12.Shaji Thomas, Preeti Nair & et al. Uncommon Presentation of common Disease, at People’s College of
Dental Science & Research Centre, People’s Campus Bhanpur, Bhopal.
13.Rajiv C. Michael Anand Jov. Indian Journal Of Otolaryngology.
14.M. Naved ,UZ Zafar, M Arif Menon Et Al,Pattern Of Cutaneous TB As Identified By Morphological
Study Of Skin Lesion At Jinnah PG Medical Centre, Karachi
15.Phillipe Katz, MD, Dana M. Hartl, MD, Phd, Agnes Guerre, MD. Clinical Ultrasound of the Salivary
Glands. Otolaryngologic Clinics of North America, Dec 2009, Vol 42(6):979
16.Kabra SK, Lodha R, Seth V. Category Based Treatment Of Tuberculosis In Children.
IJSER © 2013