The research paper published by IJSER journal is about The Healthcare Delivery Model: Rise of Wearable Medical Sensors in building EMR Applications 1
ISSN 2229-5518
The Healthcare Delivery Model: Rise of Wearable Medical Sensors in building EMR Applications
Onkar S Kemkar1 Dr P B Dahikar2
1PCD ICSR, VMV College Campus, Wardhaman Nagar, Nagpur – 440008.
*e-mail: onkarsk@in.com
2Kamla Nehru Mahavidyalaya, Sakkardara Square, Nagpur – 440009.
*e-mail: pbdahikarns@rediffmail.com
Abstract— Due to the immense volumes of medical data, the architecture of the future healthcare decision support systems focus more on interoperability than on integration. W ith the raising need f or the creation of unified knowledge base, the federated approach to distributed data warehouses (DW H) is getting increasing attention.
In this paper we investigate the important requirements of communication architecture of wireless sensor networks, Furth er, we present a federated DW H model which enables the interoperability between heterogeneous and distributed medical IS, This paper reports o n an ongoing research on developing an agent based system architecture for wireless sensor networks. The main objective of this system is to facilitate the design, implementation, and maintaining applications for sensor networks that consist of wireless sensor nodes .
Keywords— ehealth, e-records, health informatics, EMR, EPR
1. INTRODUCTION
It is estimated that the patient’s access to his own medical records and treatment information in the future will play an important role in managing treatment of chronic diseases and protecting patients’ [1]. Shared access to electronic health records will thus be important for obtaining electronic collaboration, both for the patient and also for the health care professionals.
Various types of technologies are in use by health care industry plays a vital role in improving patient- physician relationship [2].
eHealth is an overarching term used today to describe the application of information and communications technologies in the health sector. It encompasses a whole range of purposes from purely administrative through to health care delivery. For example: within the hospital care setting, eHealth refers to electronic patient administration systems; laboratory and radiology information systems; electronic messaging systems; and, telemedicine -- teleconsults, telepathology, and teledermatology.
A fundamental building block of all these applications
is the Electronic Health Record, which allows the sharing of necessary information between care providers across medical disciplines and institutions. Other important uses of eHealth are found in the areas of continuous medical education and public health awareness and education.
Also the basic health information, such as demo- graphic and health insurance information and lists of conditions, medications and allergies in EHR play the main key in medial diagnose and therapy [3].
Now consider the different options available as far as
the healthcare service provider software & healthcare
tertiary caregivers are concerned:
The patient is mobile and its health travels with him.
Healthcare services should be available pervasively,
integrated into the patient’s environment.
Mobile Grids can provide an infrastructure for an
efficient development, provision and maintenance of complex e-health applications.
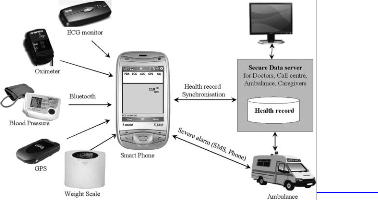
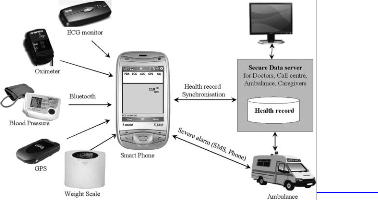
Recent advances in information and communication technologies (ICT), miniaturization of sensor devices and computers, as well as the wider availability of
connectivity and wireless networks gives rise to a number of services and applications involving wirelessly connected sensors and actuators in a body area network (BAN), personal area network (PAN) or in the environment.
Connectivity between medical sensors/devices,
gateways/hubs and healthcare services is present.
Health professionals rely on accurate data coming
from certified devices. Patient safety is most important,
but privacy is also taken care of, as required by legislation (EU Directive 46/95, HIPAA, etc.).
The aim of this work is to present an easy accessible and portable EHR with providing a robust and
IJSER © 2012 http://www.ijser.org
The research paper published by IJSER journal is about The Healthcare Delivery Model: Rise of Wearable Medical Sensors in building EMR Applications 2
ISSN 2229-5518
comprehensive support system based on embedded system design. In this case the design of embedded EHR includes integrated communication submodules based on SMS, internet and Zigbee technologies to provide accessibility of the system.
In addition to that the work provides different methods to capture and access patient’s medical records by the help of different communication media. In this
scenario, a patient’s medical record is stored in one geo- graphical location on a server which is accessible from anywhere in the world via the internet.
2. BACKGROUND
Review of literature
"Management of Health Risks" and Patient Safety is one of the cornerstones to assure policy support for the European Commission FP7 eHealth research topics [8]. Emergency response systems are one of the significant factors of safety healthcare management. There are thus several proposed prototypes and developed projects on the topic. A scalable emergency medical response system that couples the efficient data collection of sensor networks with the flexibility and interoperability of a web services architecture [9]. A wireless medical monitoring system which is capable of receiving and processing the pulse-oximetry signals from one or several monitored patients[10]. An Intelligent Healthcare Monitoring for the Homecare Scenario using multi-service architecture [11]. Akogrimo E-Health [10] deployed Heart Monitoring and Emergency Scenario on the Mobile Grids. A wireless infrastructure intended for deployment in emergency medical care, integrating low power, wireless vital sign sensors, PDAs, and PC-class systems [12].
In general, the existing approaches focus on the
protocols of data collection from sensor network and the communication between components to process data, mostly using agent technology, and to deploy the presentation data in mobility devices. These approaches thus could not deal with ad-hoc analysis to recognize the pattern-based data trends. With the use of federated DWH combined with the Sense & Response loop, our approach could process the adhoc query in the acceptable response time.
Ferreted DWH for interoperability in health
care environment
Having relevant information available to patients for management of their medical conditions still one of the main problems in medical practice. Personal health re- cords are important for patients, their physicians and the health care system [4]. Most of the patients receive their healthcare from multiple providers. Hospitals,
physicians, recovery centers, laboratories, pharmacies and health insurance institutions have their own, isolated patient records. Therefore, they can keep only a fragmental knowledge about the patient’s health condition.
Due to the high confidentiality of healthcare data and
the privacy policy of participating organizations, we propose a collaborative system (federated DWH) instead of an integrated system approach (physical DWH) for joining of distributed data assets. Rather than duplicating the sensitive data into a centralized DSS, a federated DWH virtually ties together network providers so that fundamental operational, analytical and research activities can be efficiently realized.
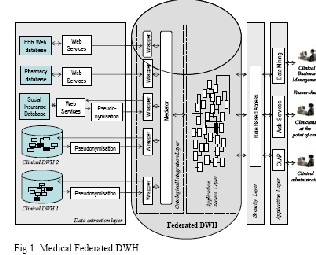
In our model (Fig.1) the different medical treatment domains, the social insurance domain, the pharmaceutical domain and the EBG repository participate in one federation. Some of them communicate with the federation via web services; others may transfer their sensitive data directly to the federation, in case of a federated query. Since only a unique interpretation of the joined data should exist, it is necessary to have a unique common federated schema. As shown in Fig. 1, the essential part of the model is the ontological integration layer. Wrappers and mediators [5], [6] are the main architectural components of a mediated query system. Participating organizations use internationally adopted standard message formats for transmission of their health information to the federation. Such standards (e.g. HL7 [7], ENV 13606, openEHR) set the structure and data types required for
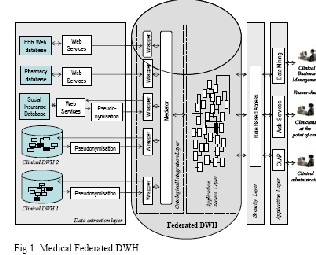
seamless integration between the systems.
3. SYSTEM DESIGN
IJSER © 2012 http://www.ijser.org
The research paper published by IJSER journal is about The Healthcare Delivery Model: Rise of Wearable Medical Sensors in building EMR Applications 3
ISSN 2229-5518
Agent based architecture
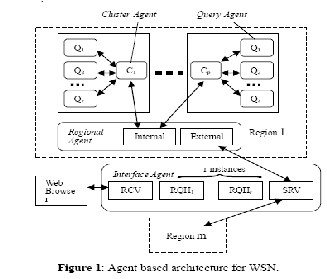
The proposed agent based system architecture is based on hierarchical software agents and classified into different types of agents based on their functionalities [13], as shown in Figure 1. The sensor network is divided into several regions due to spatial, topological, and deployment conditions. Moreover, each region is divided into several clusters based on queries, motes hardware, and data acquisition mechanisms.
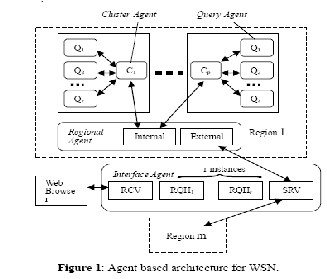
The architecture is based on a four layer hierarchy of software agents. At the interface layer of the architecture, an interface agent interacts with the sensor network. At the regional layer, the regional agent acts as a gateway between the sensor network and the traditional networks. At the cluster layer, the cluster agent performs query dissemination and efficient in- network processing. Finally at the query layer, the query agents which are located on the data collecting sensor nodes perform data acquisition and local computation.
Wireless sensor networks communication architecture
Wireless sensor networks consist of individual nodes that are able to interact with the environment by sensing or controlling physical parameters. These nodes have to collaborate to fulfill their tasks. The nodes are interlinked together and by using wireless links each node is able to communicate and collaborate with each other.
As shown in Figure 1, the wireless sensor network and the classical infrastructure comprises of the standard components like sensor nodes (used as source, sink/actuators), gateways, Internet, and satellite link, etc.
Proposed system
The study shows that existing EHR systems are well suited to receive sensor data. The three main EHR systems in Norwegian hospitals are all supported with application programming interfaces (APIs), enabling external vendors to add modules. These APIs are sufficient to implement modules for receiving sensor data. However, none of the systems currently have commercially available modules for receiving such data.
In this section we will talk about the proposed system in which we will going to discuss what type of sensors we are using, how they will read the data and, how we will store that data in the database:
If there is no clinician to interpret the data from the
sensors, questions arise concerning how to translate raw data from sensors into meta-data that is useful for clinical decision-making. Additional issues arise relating to maintenance and calibration of the sensors. While programs exist for these activities in hospitals, they do not ordinarily exist for in-home or ambulatory monitoring systems. Data aggregation and data fusion techniques can be used to overcome individual sensor calibration issues and improve confidence in observations that are derived from multiple sensors. The specifications are intended to permit on-body sensors or in-home health monitoring systems to transfer different types of data to an EHR, either directly or via an information exchange. Given the recent developments, we report on part of a project which investigates the integration of data from sensors with an electronic health record.
4. CONCLUSION
Next generation pervasive computing domains will be made up of an abundant of autonomous: processing, communicating and sensing devices. These may include personal digital assistants (PDA) wireless sensor networks (WSN) or of a medical patient centric importance, Body Area Networks (BAN). Before any data management or Information System task may be executed, the context or situation of the user and their environment needs to be taken into account. This large paradigm shift from centralized decision making networks to remote autonomy creates new challenges within the data management information quality community. In particular, how to collect, correlate and disseminate this new information pool in an intelligent
IJSER © 2012 p://www.ijser.org
The research paper published by IJSER journal is about The Healthcare Delivery Model: Rise of Wearable Medical Sensors in building EMR Applications 4
ISSN 2229-5518
manner to help support our medical decision support systems (DSS).
Data fusion and aggregation techniques may be
required for improving the degree of confidence in the extent to which the data from any particular sensor can be relied upon. In addition, it seems likely that standards will play a key role in ensuring the quality of data from different types of sensors.
ACKNOWLEDGEMENT
The author wish to acknowledge the help received from Dr D A Deshpande, Director, PCD Institute of Computer Studies and Research, VMV College campus for various inputs & methodological techniques in telemedicine.
REFERENCES
[1] Coulter, A., S. Parsons, Conference on Health Systems: “Where are the patients in decision- making about their own care?”, World Health Organization, 2008
[2] R. Shetty, “Portable Digital Personal Health Record: To Bridge the Digital Gap in Medical Information Storage of Individuals with Personal Health Records in Flash Drives,” The Internet Journal of Health, Vol. 5, No. 2, 2007.
[3] L. Moreno, S. Peterson, A. Bagchi and R. af Ursin, “Per-sonal Health Records: What Do Underserved Consumers Want?” Mathematica policy research, No. 4, May 2007.
[4] Institute of Medicine, “The Computer-Based Patient
Record,” National Academy Press, Washington, D.C.,
1991.
[5] Stolba N, Nguyen M. and Tjoa A M. Towards a
DWH Based Approach to Support Healthcare Knowledge Development and Sharing, submitted for the publication at 2007 IRMA Int. Conference, Vancouver, Canada, May 2007.
[6] Beneventano D, Bergamaschi S, Guerra F and Vincini M. Synthesizing an Integrated Ontology, IEEE Internet Computing Magazine, September- October 2003, 42-51.
[7] Heitmann KU. Kommunikation mit HL7 Version
3 – Aspekte der Interoperabilität im
Gesundheitswesen, Datenbank Spektrum,
17/2006, dpunkt.verlag, pp. 12-16.
[8] eHealth 2006 Workshop. http://www.ehealth- forsafety.org/workshops/bio_medical%202006/bi o_medical_index.html.
[9] Hashmi N, Myung D, Gaynor M and MoultonS. A Sensor-based,Web Service-enabled, Emergency Medical Response System, EESR ’05: Workshop
on End-to-End, Sense-and-Respond Systems, Applications, and Services.
[10] Morón J, Casilari E, Luque1 R, Gázquez A: Wireless Monitoring System for Pulse-oximetry Sensors, Proceedings of the 2005 Systems Communications (ICW’05)
[11] Hein A, Nee O, Willemsen D, Scheffold T, Dogac
A, Laleci G. SAPHIRE - Intelligent Healthcare Monitoring based on Semantic Interoperability Platform - The Homecare Scenario ,1st European Conference on eHealth (ECEH’06).
[12] D. Malan, T. Jones, M. Welsh, S. Moulton: CodeBlue: An Ad Hoc Sensor Network Infrastructure for Emergency Medical Care, International Worksh
[13] E. Shakshuki, H. Ghenniwa and M. Kamel, “Agent-based System Architecture for Dynamic and Open Environments”, Journal of Information Technology and Decision Making, 2(1), pp. 105-
133, 2003.
IJSER © 2012 http://www.ijser.org