International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 243
ISSN 2229-5518
Hospital Engineering and Infection
Control
Dr Sameer Mehrotra, Dr R K Ranyal, Dr Punit Yadav, Dr Sunil Basukala
Abstract: The hospital design has an important role in the control of hospital associated infections. The physical design of hospital is an essential component of a hospital’s infection control strategy, incorporating infection control issues to minimise the risk of infection transmission. Hospital design therefore, needs to consider the separation of dirty and clean areas, adequate ventilation, lighting, storage facilities and design of patient accommodation areas, including adequate number of wash hand basins and single bed facilities. However, there is inherent difficulty in establishing these fact because of too many confounding factors in the form of type of patients, man power available in the facility, the policies and procedures and other resources used. These factors cannot remain constant. A review of various studies and guidelines available on the subject was undertaken. It is concluded that the hospital design does matter for infection control.
Key Words: Design; Hospital infection; Intensive Care Unit; Operation Theatre; Prevention; Ward, facilities.
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 244
ISSN 2229-5518
In 1857, Semmelvis correlated high incidence of Puerperal fever to the transmission of infection from the healthcare workers. Subsequently it was realized that it was due to lack of facilities to take care of hand hygiene.
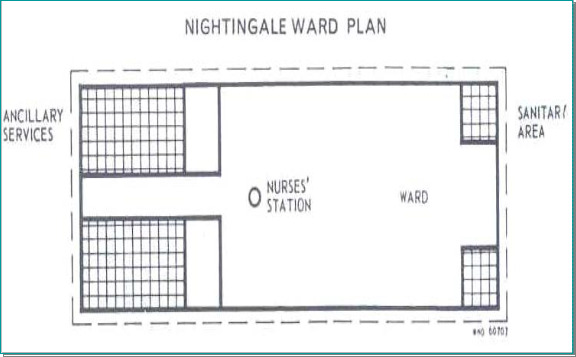
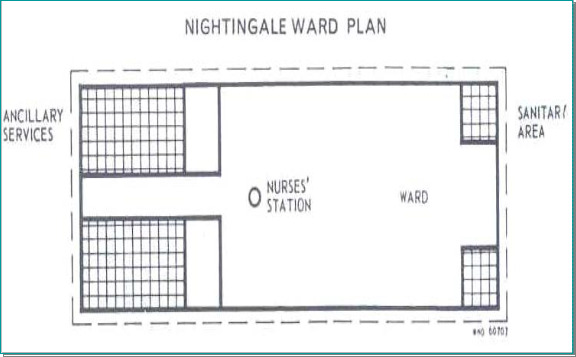
Florence Nightingale suggested a ward design (Figure 1and 2) with long corridors, central nursing
station, proper ventilation and isolation facilities. Subsequently, it was found that this ward design may result in more number of hospital associated infections. In 1875 Stephen Smith of John Hopkins Hospital made an observation that good ventilation and separation of different category of patients helps in reduction of hospital infection. In 1920 Asa Bacon of a hospital in Chicago proposed private room having toilets for the patients. In 1996 – 97, American Institute of Architects suggested that modern design of wards having single rooms is better from the point of view of infection control.
Microbial contamination of hospital environment, especially in an operating theatre and other specialized units had continued to increase prevalence of nosocomial infections. With resultant effect of high morbidity and mortality rate among patient admitted for post-operative surgery, patients in intensive care units with multi-drug resistant strains like methicillin- resistant Staphylococcus aureus (MRSA) show tedious control of these organisms. [2]
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 245
ISSN 2229-5518
The hospital design means layout of the building, functional content i.e., number and size of each department or centre and functional relationship between various areas of the same department or between different departments. It includes zoning of various departments and the design of engineering services. The objective of a hospital design is to provide safe and comfortable environment for patients, staff and visitors. It is also linked to the control of hospital associated infection. However, there is a severe degree of difficulty to establish a direct relationship between hospital design and control of hospital associated infection. It is the imbalance between classical triad of epidemiology i.e. agent, host and environment which leads to the initiation of disease process and to which hospital acquired infections are no exception. The hospital environment plays an important part in the development of infection. Whereas, the hospital may not have such control over the host factors and agents, the hospital certainly is responsible for the environment that surrounds the patients. By controlling and adequate sanitising of the environment of the host, the hospital authorities can markedly reduce the incidence of hospital acquired infections.
The type of studies which can be undertaken to find a correlation between design and infection may be based upon following:-
(a) Comparison of hospital associated infection in the similar type old and new facilities of the same hospital for example old and new wards.
(b) Design features supporting hygienic procedures for example hand washing, sanitary areas etc.
(c) Design features which are consistent with our knowledge of micro- Organisms for example absence of dado leading to accumulation of dust.
(d) Design features for which direct evidence is available for example HVAC System of hospital building.
It is of paramount importance to consider hospital infection control measures while planning
various departments like wards, operation theatre (OT), intensive care unit (ICU), central sterile supply department (CSSD), dietary, laundry etc. However, presently only ward, ICU and OT are being discussed
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 246
ISSN 2229-5518
here. The aim of this paper is to review various studies and guidelines and analyze the role of hospital design of important areas for infection control in the hospital.
A systematic review of various studies related to hospital architecture and infection control was undertaken. Certain exclusion and inclusion criteria were framed to select the articles for the study. The standard data base for searching the articles were used. Guidelines available on the subject and the search material were studied and analysed.
The design should support functional segregation of patients and their flow. It is imperative that the basic design features should not be compromised for example the space requirement for any facility. There should be adequate provision of basic amenities like sanitary areas. In a systematic review of 382 studies it was concluded that reduction in hospital infection will be there if basic conditions like availability of sufficient space, isolation capacity and hand washing facility are adequate [3]. It was observed that the compliance of practices increases if proper support is provided with the design. For example in a study it was observed that the hand washing practice increases by 25 % by increasing the bed to sink ratio from 1: 4 to 1:1. [4] In general, following design features must be kept in mind during planning of a hospital from the infection control point of view [5]:-
(a) The clean and dirty utility rooms should be planned keeping in view the future expansion.
(b) The location of utility rooms to be sited close to treatment and procedure rooms for safe and easy transportability of used and contaminated items.
(c) The instrument reprocessing activities should be planned in a separate room which may or may not be clubbed with CSSD. Rather than in a clean room or patient care room.
(d) Adequate ventilation should be provided in the dirty utility and instrument reprocessing room
(e) Instrument processing room should have adequate space and the sinks to be of large size so that the instrument may be processed without any spillage.
(f) Each examination room, procedure room, all toilets, all laboratories, medication preparation area, dirty utilities must have hand washing sinks. The hand washing soap dispensers to be located at convenient places.
(g) The environmental surfaces like walls, floors, and built in furniture should be easy to clean.
(h) Staff should be provided with adequate lounge area, for eating/ drinking so that they are not temped to eat/ drink in patient care areas, laboratories, clean area and dirty utility.
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 247
ISSN 2229-5518
(a) Public Zone: For example Lobby, waiting area, sanitary area and there should be separation of incompatible patients
(b) Joint use zone – For example reception and clinical rooms
(c) Staff zone – For example staff sanitary area and retiring rooms
The ward must have a clean utility area for keeping sterile and clean items. Similarly it should have a dirty utility area for used items and a Janitor’s closet for storage of housekeeping equipment. There should be a day room facility for patients to sit and spend the time with the visitors or amongst light entertainment. Day room reduces the movement of patients in clinical area and so helps in containing the infection. Each ward should have adequate isolation facility with ensuite shower, toilet and hand washing facility. This provides more flexibility to design.
The wet surfaces promote growth of microorganisms. Therefore, the floor material of the ward should be easy to clean and should absorb less moisture. The wall material to be clean, smooth, should not accumulate dust and absorb moisture. Walls and ceilings to have as minimum surfaces as possible. The corners at the junction of walls and floor should be coved with floor flushing and dado of about 1.2 m. The nursing station of the ward should be provided with adequate space and hand washing facilities [8].
ICU: A number of professional and scientific bodies in UK, USA and Europe have published guidelines on the design and layout of ICUs. All emphasize the importance of adequate isolation facilities (at least one cubicle for every six beds) sufficient space for each bed (20 m2), wash hand basins between every other bed, ventilation including positive and negative pressure ventilation for high risk patients, storage and utility space [9].
Health Building Note, UK recommends one wash hand basin for each bed. There should be air lock or air curtain at the entrance of the facility. Air changes to be maintained at a rate of 15 per hour. Isolation facilities to be provided @ 1-2 cubicles per 8 beds. It is observed in various studies that optimum space, adequate number of sinks isolation room facilities reduce hospital associated infection [10, 11].
(b) Zoning
(c) Design of various areas & fitments
(d) HVAC System
(e) Materials used
OT should be located close to critical care areas away from the main traffic and OPD areas. There should be zoning which is the functional segregation of OT from less clean to sterile area. Many authorities prefer to segregate OT in to following areas:
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 248
ISSN 2229-5518
(a) Disposal area (b) Protective area (c) Clean area
(d) Sterile area
The basic parameters of the environment for OT which directly or indirectly support the control of infection include:
(a) Temperature - 23 0 C + 3 0C
(b) Relative Humidity - 40 % to 60 %
(c) Total air changes per hour – 20 to 25 (d) Fresh air allowance – 10 to 15 per hour (d) Positive pressure – 25 Pa
The drains, sewage pipes and waterlines should be avoided near and above sterile zone of OT. The OT floor should be seamless as far as possible or with minimum joints. The joinery should be sealed with state of the art craftsmanship so that no uneven surface is left. The corners at the junction of walls and the floor should be rounded off. Preferably the dado should be up to ceiling height. The undue projections or sharp corners in the design of the OT should be avoided.
The ventilation system of OT should include a primary filter, a secondary filter and a final filter (99.97 %) of efficiency up to 20, 5 and 0.3 microns, respectively. American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) recommends [13] that there should be a separate air handling unit for similar level of OTs. The AC duct should be of aluminum to avoid pitting. Manometer probe should be installed for monitoring of HEPA filter clogging. Depending up on the type of surgery and level of clean environment required the ventilation system may be of different variety as given below:
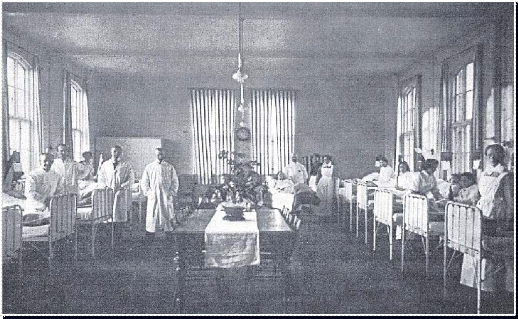
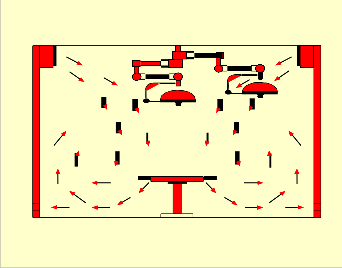
(a) Conventional type with turbulence of air (Figure 3) (b) Laminar air flow system (Figure 4)
(c) Ultra clean ventilation system (Figure 5) (d) Guided airflow ventilation system
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 249
ISSN 2229-5518
Conventional Ventilation Systems
Laminar flow Systems
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 250
ISSN 2229-5518
Ultra Clean System
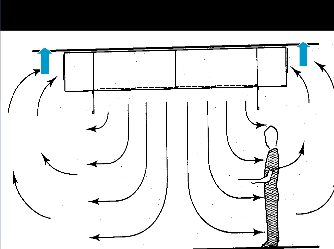
It is observed that the bacterial contamination is least in ultra clean than in laminar flow and in conventional systems [14]. Guided airflow ventilation system provides a 3 directional (vertical, horizontal and diagonal), stable and sterile airflow to create a clearly defined sterile zone for the surgery. It maintains bacteria count of 0.5 cfu /m 3 within 300 mm from wound area and less than 10 cu/ m 3 within the clean zone.
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 251
ISSN 2229-5518
should be divided into following areas: (a) Receiving area
(b) Distributing area
(c) Area for sorting dirty linen
(d) Area for sluice Machine
(e) Adequate space for other areas
The hospital design has an important role in the control of hospital associate infection. However, it
is difficult to establish an evidence linking hospital design and infection. This is because any such study has too many confounding factors which are impossible to keep constant for example type of patients, man power available in the facility, the policies and procedures and different resources used. A review of various studies and guidelines available on the subject was undertaken. It is concluded that the hospital design does matter for infection control, though it may be difficult to generate an evidence base.
1. Noskin GA, Peterson LR. Engineering Infection Control through Facility Design, Emerging
Infectious Diseases Journal, Vol. 7, No. 2, Mar–Apr 2001.
2. Singh K, Kishor K. Bacterial contamination in operating theatres of district hospital budgam in
Kashmir division. INNOVATIVE JOURNAL OF MEDICAL AND HEALTH SCIENCE. 2013;3(2).
3. Dettenkofer M. Does the Architecture of hospital facilities influence nosocomial infection rates? A
systematic review. Journal of Infection Control and Hospital Epidemiology , vol. 25 no. 1 , 2004.
4. Kaplan L M, McGuckin M. Increasing handwashing compliance with more accessible sinks.
5. AIA. Guidelines for Design and construction of hospital and health care
Facilities. Washington, DC: The American Institute of Architects and the facilities Guidelines
institutes, 2001:73, 103-127.
6. Putsep Ervin, Modern Hospital International Panning Practices, Lloyd Luke Ltd London, 1979 ;
611-12.
7. Richard A, Van E. Modern hospital design for infection control, Health care design, Nov 2006
; 26Ayliffe GAJ et of Hospital Infection A Practical hand Book , Arnold London, Fourth
Edition, 2000 ; 131-40.
8. O’ Connell NH, Humphreys H Dublin. Intensive care unit design and environmental factors in the acquisition of infection. Hospital Infection 2000 Aug ;45 ( 4 ) :255 -62.
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 4, April-2015 252
ISSN 2229-5518
9. Scottish Health Planning Note 27 : ICU, Department of Health The stationary Office NHS London, September 2000; 11-8.
10. Abraham B. Do isolation rooms reduce the rate of nosocomial infections in the Paediatric ICU,
Journal of Critical Care , 2002, 17 (3), 176
11. Laufman H, Hospital special care facilities. Academic Press Fifth Avenue New York ; 1981 : 15-30.
12. Health Technical memorandum 2025, Ventilation in Healthcare premises,NHS Estates
Department of Health, HMSO London, 2002 : 59 – 70.
13. Arlet G et al., Measurement of bacterial and fungal air counts in two bone marrow transplant
unit, Journal of Hospital Infection, 13 (1), 63-69.
14. Laboratory Biosafety Manual, World Health Organisation Geneva, Second Edition , 7-27.
a) Dr Sameer Mehrotra, MBBS MD DNB (Hospital Administration), PGDHM, Assistant Professor, AFMC, Pune-411040.
b) Dr R K Ranyal VSM,MBBS MD (Hospital Administration), Prof and Head of Department, AFMC, Pune- 411040
c) Dr Punit Yadav MBBS MD (Hospital Administration), Professor, AFMC, Pune- 411040
d) Dr Sunil Basukala, MBBS, Resident MD (Hospital Administration), AFMC, Pune- 411040
Addresses
Department of Hospital Administration, AFMC, Pune- 411040
a) Dr Sameer Mehrotra - +91 8552 081 940 b) Dr R K Ranyal - +91 9168819977
c) Dr Sunil Basukala - +91 8412 094 782
a) | Dr Sameer Mehrotra | |
b) | Dr R K Ranyal VSM - | |
c) | Dr Punit Yadav | |
d) | Dr Sunil Basukala | - anyurysm@gmail.com |
IJSER © 2015 http://www.ijser.org