International Journal of Scientific & Engineering Research, Volume 4, Issue 11, November-2013 1015
ISSN 2229-5518
Food poisoning in Morocco: Evolution and
Risk factors
Hajar Rebgui1*, Nesma Nekkal1, Sanaa Benlarabi2, Fayçal El Hattimy1, Fatine Hadrya1, Abdelmajid Soulaymani1, Rachida Soulaymani-Bencheikh2, 3,, Abdelrhani Mokhtari1
1Laboratory of Genetics and Biometry, Faculty of Sciences, University Ibn Tofail, Kenitra, Morocco
2Moroccan Poison Control and Pharmacovigilance Center, Rabat, Morocco
3 Faculty of Medicine and Pharmacy, University Mohammed V, Rabat, Morocco
*Corresponding Author Email address:rebgui.hajar@gmail.com
Abstract—In order to contribute in reducing the morbidity and the mortality resulting from food poisoning in Morocco and improving the treatment of patients, this study is an analysis of the current situation of this pathology over a period of five years. This analysis consists of describing the different characteristics linked to food poisoning cases recorded in the Anti Poison and Pharmacovigilance Center of Moroc- co (CAPM) between 2007 and 2011 in Morocco, as well as identifying the risk factors that are related to these cases. During the study pe- riod, 6 960 poisoning cases have been collected, included 24 deaths. The average age of patients was 24 years. The two sexes were af- fected in the same way. The males were more exposed to fatal poisonings. Meat and meat products were the most incriminated. However, the fatal poisoning was mainly linked to dairy products. The urban areas were the most affected, while the rural areas were more exposed to fatal poisonings (RR=5, p<0,001). The majority of reported cases had showed clinical signs from which the most frequent ones were disorders in the gastrointestinal system (89%).
Index Terms— Food poisonings, pathology, risk factor, CAPM.
—————————— ——————————
1 Introduction
The development and the increase of the number of commercialized food products make food poisoning (FP) a more com- mon disease in all countries. This disease causes human sufferings and significant health costs [1]. The contribution of anti- poison centers in the treatment of FP is clear. According to a study of Harrison and al, these centers reduce significantly the costs related to the treatment of these diseases [2, 3, 4].
The epidemiological situation in some countries
In the United States, 76 million of food poisonings (26 000 in 100 000 residents) from which 325 000 persons were hospital-
ized (111 in 100 000 residents) and 5000 persons died (1,7 in 100 000 residents) [5]. In the United Kingdom, in 2000, the number
of poisonings increased to 2 million (nearly 3400 in 100 000 residents). The involved bacteria was: Campylobacter jejuni (77,3%),
Salomnella (20,9%), Escherichia Coli O 157 : H7 (1,4%) and all others (<0,1%). In France, in 250 000 to 750 000 food poisonings per
year (400 to 1210 in 100 000 residents) , 70 000 were subject to emergency consultation (113 in 100 000 residents), 15 000 persons
were hospitalized (24 in 100 000 residents) and 400 persons died (65 in 100 000 residents).
The epidemiological situation in Morocco
A gradual increase in the last ten years has been noticed. Indeed, the number of FP cases and episodes doubled from 1996 to
2001. In Morocco, the FP cases represent 11% of poisonings. More than 90% of FP cases are caused by confirmed or probable
bacteria. Approximately 7% cases have a chemical cause: food contamination especially by pesticides. Nearly 1% of FP cases are
of plant cause (Addad). The rest had an unidentified cause (1,5%) [6]. Food contamination can come from raw materials or food
processors. Water supply can also be a cause of FP. The FPs are under-reported in Morocco as in many countries of the world.
Since the Moroccan population had not known the FP risks, these FPs are reported only in aggravated cases. Thus, we can esti-
mate 10 cases for each report [7]. In order to contribute in reducing the morbidity and the mortality resulting from food poison-
ings in Morocco and improving the treatment of patients, this study is an analysis of the current situation of this pathology over
a period of five years. This analysis consists of describing the different characteristics linked to food poisoning cases recorded in
the Anti Poison and Pharmacovigilance Center of Morocco (CAPM) between 2007 and 2011 in Morocco, as well as identifying
the risk factors that are related to these cases.
2 Data and methods
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 11, November-2013 1016
ISSN 2229-5518
This is a retrospective study over a period of 5 years (from 2007 to 2011) that concern 6960 food poisonings cases reported to the Anti Poison and Pharmacovigilance Center of Morocco (CAPM).
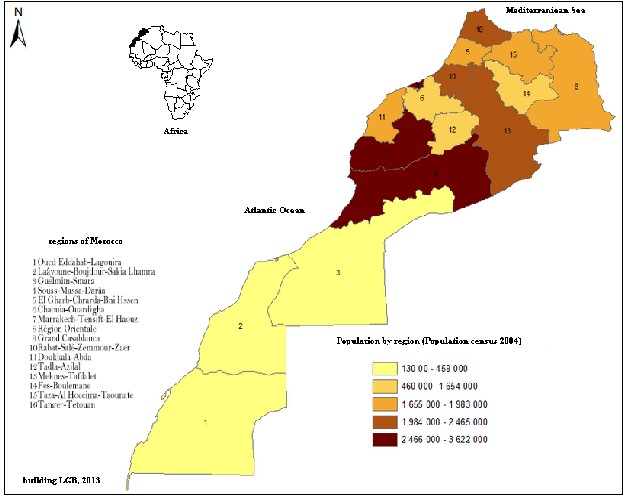
Morocco is bordered in the East and in the Southern East by Algeria, in the South by Mauritania, in the West by the Atlantic Ocean and in the north by the Mediterranean Sea. Morocco has a surface area of 710 850 Km², and in the administrative level, it is divided, according the Dahir NO -97-84 of 23 Dhu al-Qa'da 1417 / 2 April 1997, into sixteen regions (fig 1). Morocco had a population of 29 680 069 inhabitants in 2004 [8]. The country is generally characterized by a mild and temperate climate, with a humid and cold winter, and a dry and hot summer. The thermal variations are sometimes brutal. The irregular and heavy rain- falls are concentrated in short periods, with an alternation in the period of floods and the period of droughts [9].
Moroccan people have a very varied alimentation. Cereals are the base of their alimentation, followed by fruits and vegetables, and then beef and game meat [10].
All data of poisoning report sheets, filled in by the doctor in charge of the case or, failing that, by the nurse, coming from health facilities (in sixteen Moroccan regions) to the Toxicovigilance unit of the center regularly, and data of medical files filled in according to telephone responses by the CAPM doctor of the Toxicological information unit, were entered in a special data- base and then submitted to treatment. For data processing, we have used some descriptive tools such as the frequencies and the specific lethality rates (refers to the link between the recorded deaths as a result of a poisoning and the total number of poison- ing cases, and it is specific to a given modality). The description of the sample concerned the characteristics of the poisoned population (year, sex, age, origin, type of poisoning, symptoms, clinical signs, gradation and evolution) and the characteristics related to the suspected food. The studies and the associations between the dependent variable (evolution: cure/death) and all these characteristics were tested, particularly by the chi-square test (represented by it signification p) and the estimation of the relative risk (RR) for a joint analysis of the two variables. The gravity evaluation is done by the Poisoning Score Severity (PSS) [11]. Vector foods were classified according to Codex Alimentarius done by the Anti Poison and Pharmacovigilance Center of Morocco [12].
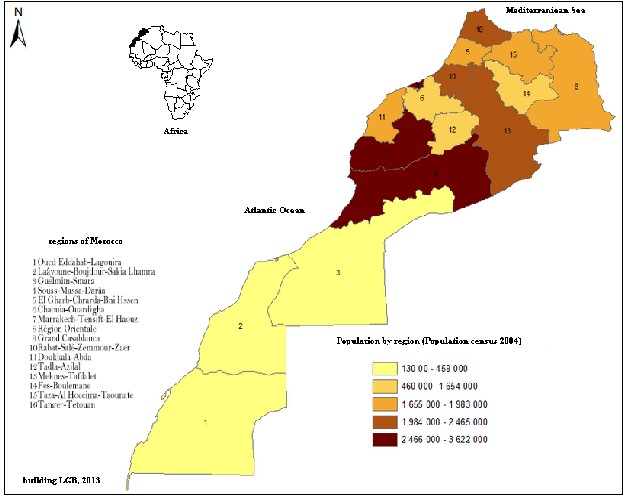
Fig 1: Distributionof the Moroccan population according to the General Census of the Population
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 11, November-2013 1017
ISSN 2229-5518
3 Results
3-1 Characteristics of the poisoned population
The average annual number of reports was of 1392 cases. The year 2009 had recorded the minimum of cases, namely 1074
cases, while the year 2010 had recorded the maximum of cases, namely 2075 cases (Fig 2). The seasonal distribution shows that
more than the third of food poisoning diseases was noticed in summer with a specific lethality of 0,32%. This increase may be
justified, on the one hand, by the role of temperature in the spread of germs in foods and water, and the increased consumption
of fruits and vegetables during this period of year, and on the other hand, by poor preservation of food. The geographical distri-
bution of the cases shows that all the regions were affected, with a maximum of declarations was recorded in the region of Mar-
rakech-Tansift-AlHaouz (1 160 cases), followed by the region of the Oriental (1 009 cases) .The age group that is superior to 15
(>15) was the most affected with 59,8 and a lethality of 0,3%. The average age of patients was 24 years. The distribution accord-
ing to sex showed that both sexes were affected in the same way. Males were the most exposed sex to lethal poisonings with a
specific lethality of (0,46%). Patients of urban origin were the most affected (76,8%). The highest specific lethality was recorded
in patients of rural origin. This may be explained by the lack of health infrastructures and means of communication (telephone,
Fax…) as well as the absence of food hygiene in rural areas. The FPs were frequent at home with 65,7%. Most of poisoning cases
were collective (57,0%) with a specific lethality of 0,48%. The severity of patients’ health status was often moderate (level 25; 765
cases), probably due to the mildness of the created diseases (often considered as transient). Complications appeared in 176 cases
(level 3). The fatality was noticed in 24 cases (level 4). The progression was positive in 99 % of cases. 28 cases had after-effects
and 24 cases died (a lethality of 2,9%). Most of reported cases had symptoms (namely 87%) (Table 1). According to the results of
the analysis, almost all cases had disorders in the gastrointestinal system (89%), associated or not with disorders in the central
and peripheral nervous system (7%) and general disorders (2%). Other disorders were shown at low frequencies. The gastroin-
testinal system’s most frequent disorders were vomiting, abdominal pain, nausea and diarrhea (Table 2).
Fig 2: Distribution of poisoning cases by years and months
Table 1: Epidemiological characteristics of the study population
Epidimological Para- metrs | Global | | Evolution | | Specific Lethality (%) |
| Numbers (N=6 960) | Percentage (100 %) | Cured (N=5 890) | Deceased (N=24) | |
Age groups >15 years ≤ 15 years Active n | 4 164 2 299 6 463 | 59,83 33,03 92,89 | 3 508 1 926 5 434 | 13 4 17 | 0,31 0,17 |
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 11, November-2013 1018

ISSN 2229-5518
Sex Male Female Active n
3 326
3 257
6 583
47,79
46,80
94,59
2 687 15
2 865 6
5 552 21
0,46
0,18
Origin Urban Rural Active n
5 349
1 429
6 778
76,85
20,53
97,38
1 190 9
4 562 11
5 752 21
0,17
0,77
Place ofpoisoning
Home
Job
Public
Other
Active n
4 573
570
1 654
49
6 846
65,70
8,19
19,45
0,70
94,04
3 852 9
528 2
1 192 9
40 -
5 612 20
0,20
0,35
0,66
0,0
Type ofpoisoning
Isolated
Collective
Active n
3 971
2 988
6 959
42,93
57,05
99,98
2 448 5
3 442 19
5 890 24
0,17
0,48
Season Autumn Winter Spring Summer Active n
1 452
1 009
1 859
135
4 455
20,86
14,50
26,71
35,99
98,06
1 260 1
837 3
1 607 3
2 074 8
5 778 15
0,07
0,30
0,16
0,32
Clinical status Symptomatic Asymptomatic Active n
6 083
876
6 959
87,40
12,59
99,99
5 190 12
700 12
5 890 24
1,37
0,20

Gradation None (Level 0) Minor (Level 1) Moderate (Level 2) Severe (Level 3) Fatal (Level 4) Active n
185
510
5 765
176
24
6 660
2,66
7,33
82,33
2,53
0,34
95,19
175 -
462 -
5 034 -
132 -
24 24
5 827 24
-
-
-
-
100,0
Table 2: Distribution of the clinical signs of the poisoned cases by effects’ categories according to the system or the concerned organ


Effect’s categories according the system or the organ | Number | | % |
Disorders in skin and its adnexa | 27 | 0,60 |
Disorders in the musculoskeletal system | | 3 | <0,1 |
Disorders in the central and peripheral nervous system | 312 | 6,89 |
Disorders in the visual system | | 2 | <0,1 |

IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 11, November-2013 1019

ISSN 2229-5518
Psychiatric disorders 2 <0,1
Disorders in the gastrointestinal system 4 026 89,0
Disorders in the general cardiovascular system 4 0,1
Disorders in heart rate and rhythm 30 0,66
Disorders in the respiratory system 24 0,53
Disorders in the red bloodline 1 <0,1
Disorders in the general condition 97 2,14


Active n 4 528 100,00
3-2 Characteristics linked to the suspected food
According to the Codex Alimentarius classification, meat and meat products (11,9%) were on top of the most incriminated food, followed by fish products (8,0%) and dairy products (7,3%) (Table 3).
Table 3 : Distribution of the poisoned cases according to the nature of the suspected food

Food categories
The dominance of meat products in the poisoning may be explained by the fact that meat is a good place for the growth of most microorganisms, and that because of the non-respect of health conditions principally, especially in the slaughterhouses during the slaughter phase. The poisoning may also occur if the meat is eaten raw, undercooked or recontaminated after cook- ing. The suspected food products in lethal poisoning were mainly dairy products (6 cases) and fruits and vegetables (5 cases). However, the highest lethality was noticed in cases of poisoning by fruits and vegetables (SL=2%).
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 11, November-2013 1020
ISSN 2229-5518
3-3 Study of the influence of epidemiological variables on the prognosis of patients
Factors influencing the prognosis of poisoned patients are illustrated in table 4.
Table 4: Factors influencing the prognosis of poisoned patients
Variable (Modality 1 vs Modality 2) | Evolution (Cured vs De- ceased) | RR [CI 95%] | P |
Sex (Male vs Female) | 5 552 vs 21 | 2.66 [1.03-6,88] | 0,047 |
Origin (Rural vs Urban) | 5 752 vs 20 | 4.68 [1.93-11.33] | 0,001 |
Significant link (5 %) ; 0,001 < p ≤ 0,01 : very significant link (1 %). RR : Relative risk ; CI 95 % : confidence in- terval at 95 %. |
On the six studied variables (sex, age, origin, poisoning type, clinical status, symptoms), it turned out that males were the most affected and that the difference between the two sexes is significant (x2=4,443, 0,01 < p ≤0,05). Men are twice more likely to progress to death than women (RR =2,666; CI 95 % : 1,033-6,880).
Poisoned patients in rural areas are four times more likely to progress to death than those who are poisoned in urban areas (RR= 4,686 ; CI 95 % : 1,937-11,333). This may be explained by the increased consumption of fruits and vegetables, that are often unwashed, by the inhabitants of rural areas on the one hand, and on the other hand by the poor preservation of food (lack of refrigerators and storage equipments).
4 Discussion
Food poisonings are considered to be an everyday growing public health problem whether in developed countries or in de- veloping countries [1, 13, 14]. In Morocco, according to data from CAPM, the FPs occupy the first position (22,1 %) of all poison- ings, apart from scorpion infections and stings [15]. During the period from 1992 to 2009, 17 896 FP cases were reported to the CAPM including 59 deaths. For most people they are sporadic and minor and often are unnoticed by health professionals or patients. Therefore, only 6960 FP cases were reported to the CAPM over five years including 24 deaths.
This figure does not reflect the reality since in France, between 2001 and 2003, there was 1656 episodes of FP reported includ- ing 22113 patients and 11 deaths of whom 60% had a salmonella origin and 65% occurred in institutional catering [16]. World- wide, 2,1 million adults and 3 million children die because of the consumption of water or contaminated food [13,17]. In the United States, in 1994, an outbreak of salmonellosis due to ice cream affected 224000 persons [17]. The disparity of the epidemio- logical situation of FPs is due to changes in people’s lifestyles and the behavior of microbial germs [1,17].
In our series, as in literature, the FPs are more and more common due to the change in lifestyle (preparing food long before consumption because of women’s work outside the house, buying pre-prepared food…), food habits (preparation of leben from raw milk left exposed to open air for a few days…), the intense development of informal sales sector as well as the new agri- food technologies.
As for the frequency, the urban areas occupy the first place: this is related to the overcrowding in urban areas and the access to health facilities. The FP phenomenon is seasonal with an increase in summer and spring. This is explained by the important role of temperature in the spread of germs in food and water, the increased consumption of fruits and vegetables during these seasons as well as people’s movements especially in summer (holidays, outings, trips…). The FPs affect male adults/city- dwellers at home. This is probably related to rural exodus of the population of young men who live alone and eat anyhow be- cause of their low purchasing power. Meat and meat products (11%) was on top of the most incriminated food, followed by fish products (8%) and dairy products (7%): in fact they are easily perishable and can be contaminated by chemicals. The microbio- logical risks and the FPs they cause are considered as a growing health problem. In many countries, we noticed in the last dec- ades significant increases of the negative impacts of diseases caused by microorganisms transmitted mainly by food, such as Salmonella spp and Campylobacter spp. New serious threats emerged in the food chain such as the enterohemorrhagic Escherichia coli and the bovine spongiform encephalopathy (BSE). In addition to that, the chemical risks remain as an important source. Among chemical contaminants in food, we can mention natural toxicants such as mycotoxins and marine toxins, environmental contaminants such as mercury and lead, and substances that exist naturally in plants. Food additives, micronutrients, pesticides and veterinary drugs are deliberately used in the food chain. However, we must make sure that their use is safe [18]. Clinically,
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 11, November-2013 1021
ISSN 2229-5518
the affection of the gastrointestinal system was normal in this series. We note that diarrhea is also a main cause of the malnutri- tion of infants and young children. The high prevalence of diarrheal diseases is a sign of implicit major problems of food safety [1, 13]. Generally, the evolution was favorable with some deaths whose number was significant though.
5 Conclusion
The number of reported FP was almost stable between 2007 and 2001, while in 2011, a remarkable decrease was noted. This may be related to the efforts made by the Anti Poison and Pharmacovigilance Center of Morocco and the organization of many open days of awareness on the dangers of food poisonings, health education, information and communication regarding food hygiene. The institutional catering shall require a regular monitoring and particularly households in which FPs had occurred previously. We must be aware that each reported FP limits its aggravation. We must also make extra efforts to improve the epi- demiological system of investigation.
References
[1] D. Malvy, F. Djossou, L. Bras, "Infections et toxi-infections d’origine alimentaire et hydrique: orientation diagnostique et conduite à tenir," EMC Pathologie professionnelle et de l’environnement, pp. 276-284, 2003.
[2] A. Khattabi, N. Rhalem, R. Soulaymani-Bencheikh, "Centre Anti Poison et de Pharmacovigilance du Maroc : naissance, défis et promesses," Toxico- logie Maroc, no.1, pp.3-7, May 2009.
[3] D.L. Maj, M.C. Harrison, R.D. Jolaine, K.S. Marion, P.C. Langley, " Cost-effectiveness of Regional Poison Control Centers," Arch Intern Med, vol.156, no.22, pp.2601-2608, 1996.
[4] E. Zaloshnja, T. Miller, P. Jones, T. Litovitz, J. Coben, C. Steiner, "The Potential Impact of Poison Control Centers on Rural Hospitalization Rates for
Poisoning Pediatrics", vol. 118, no. 5, pp. 94-100, Nov 2006.
[5] Organisation mondiale de la Santé (OMS), "Salubrité des aliments et maladies d’origine alimentaire", Aide Mémoire no. 237. 2007.
[6] K. Benkaddour, "Situation épidémiologique des toxi-infections alimentaires collectives au Maroc, 1992-2001. Séminaire national sur l’application du système HACCP dans le domaine de l’hygiène alimentaire". Ministère de la santé, pp. 2-111, 8-10 May 2002. (Conference proceedings).
[7] S. Benlarabi, I. Semlali, G. Eloufir, M. Badri, R. Soulaymani Bencheikh, "Les toxiinfections alimentaires collectives: données du centre Anti Poison et de Pharmacovigilance du Maroc", Premier Congrès National de la Société Marocaine de Toxicologie Clinique et Analytique, pp.78, 10-11 March 2006. (Con- ference proceedings).
[8] Haut Commissariat au Plan, "Recensement Général de la Population et de l'Habitat. Caractéristiques démographiques et socio-économiques de la population marocaine", (URL : http://www.hcp.ma/Recensement-General-de-la-Population-et-de-l-Habitat_a92.html 2004).
[9] M. Cherbi, S. Lek, A. Arab, "Distribution du Zooplancton dans les lacs à climat chaud méditerraneén", Compte Rendu Biologie, vol. 331, pp. 692-
702, 2008.
[10] M. Monkachi, "L’augmentation traditionnelle dans les compagnes du Nord du Maroc", Médiévale, vol. 33, pp. 91-102, 1997.
[11] H.E. Person, G.K. Sjöberg, J.A. Haines, "Poisoning Severity Score. Grading of Acute. Poisoning". Clin Toxicol, vol. 19, pp. 205-213, 1998.
[12] L. Aoued, S. Benlarabi, R. Soulaymani–Bencheikh, "Maladies d’origine alimentaire Définitions,Terminologie",Classifications.Toxicologie Maroc, vol.
6, no. 3, pp. 3-6, 2010.
[13] N. Gausserès, J. Fricker, "Toxicologie alimentaire: Pathologie professionnelle et de l’environnement", EMC, vol. 201, pp. 125-131. 2003.
[14] L. Ouammi, N. Rhalem, R. Aghandous, I. Semlali, M. Badri, J. Jalal, "Centre Anti Poison et de Pharmacovigilance du Maroc : Profil épidémiologique des intoxications au Maroc". Toxicologie Maroc", no. 1, pp. 8-13, 2009.
[15] G. Delmas, F. Le Querrec, F.X. Weill, A. Gallay, E. Espié, S. Haeghebaert, V. Vaillant, " Les toxi-infections alimentaires collectives en France en 2001-
2003", (URL : www.invs.sante.f, 2006).
[16] Organisation mondiale de la Santé (OMS), bureau régional du pacifique occidental comité régional, "Sécurité sanitaire des aliments. Shanghai",
2004.
[17] Organisation mondiale de la Santé (OMS) Programme Salubrité des aliments. (L’URL: http://www.who.int/fsf, 2002)
IJSER © 2013 http://www.ijser.org