The research paper published by IJSER journal is about Fatal tuberculous meningovasculitis 1
ISSN 2229-5518
Oumerzouk J, Hssaini Y, Ait Berri M, Ragabbi A, El jouehari A, A Bourazza
—————————— ——————————
Tuberculous meningitis (TBM) usually results in ischemic stroke by arteritis. The clinical picture of strokes in TBM is polymorphous. Diffusion weighted imaging (DWI) provides information regarding tissue is- chemia at an early stage allowing rapid treatment. We report in this paper, a case report of a patient present- ing a fatal tuberculous meningovasculitis.
A 45-year-old woman, previously healthy, ad- mitted to the hospital with a 15 days history of worsen- ing pancranial headache, confusion and fever with peaks at 40˚ C. She also complained of photophobia, nausea and recurrent vomiting. The neurologic symp- toms progress after 8 days to increasing weakness of the lower limbs. On neurological examination, the pa- tient was somnolent and disorientated, with bilateral sixth cranial nerve palsy and neck stiffness. Kernig's sign was positive. The patient was noted to have flaccid paraparesis (motor grade 4/5) with T8 sensory level. The deep tendon reflexes were present on the upper limbs and absent on the lower limbs. The plantar re- sponses were extensor. The cerebrospinal fluid was noted to be clear colorless and contained 10
RBCs/mm3, 560 WBCs/mm3 (96% lymphocytes), glu- cose 78 mg/dL (serum level, 229 mg/dL), protein 230 mg/dL. Contrast brain and spine MRI was unremarka- ble, but electroencephalogram showed diffuse slowing. Laboratory tests revealed hyponatremia of 125 mmol/l(normal 136-144) and CRP of 25 mg/l (nor- mal <7). Chest computed tomography scans showed bi-
lateral basal alveolar syndrome with airbronchogram
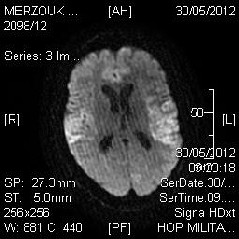
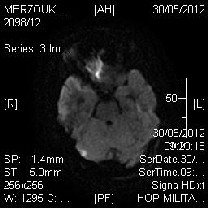
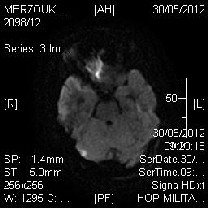
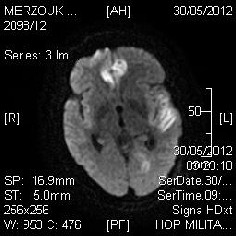
(figure 1) and real Time Mycobacteria tuberculosis PCR analysis performed on CSF was strongly positive. The patient was treated with 4 major antituberculosis and corticosteroids. Two days later, the patient presented sudden alteration of consciousness status immersing the patient in coma (GCS = 7). The patient was admit- ted in intensive care unit, where, performed brain MRI showed corticosubcortical T2-Flair and Diffusion weighted hyperintense lesions within frontal lobe (figure
2), temporal lobe (figure 3) and right cerebella hemi- sphere (figure 4), with contrast enhancement. The
IJSER © 2012
whole was suggestive of disseminated cerebral vascu- litis complicating tuberculosis infection. Unfortunately, despite a heavy treatment, the patient went into deep coma and passed away by cardiac arrest, 5 days after her intensive care unit admission.
Ischemic involvement of small and medium sized vessels at the base of the brain is a common complication in tuberculous meningitis (TBM).1TBM usually results in ischemic stroke but rarely it may result in hemorrhagic infarcts that are attributed to both arteri- al and venous thrombosis.2 Stroke in TBM occurs in 15–
57% of patients. Many factors simultaneously play a role in its occurrence: stage of meningitis, hypertension, hydrocephalus, and exudates.3Most infarcts in TBM are as a result of hemodynamic hypoperfusion due to a var- iable combination of vasospasm, intimal proliferation and thrombosis of cerebral blood vessel walls 1. It is re- garded as a poor prognostic predictor of TBM.2
The pathophysiological mechanisms implicated in cere- bral vasculitis are diverse and can include: a direct pathogenic effect of the infectious agent on the vessels, role of cytokines (tumor necrosis factor, vascular endo- thelial growth factor and matrix metaloproteineases) in damaging the blood brain barrier, immunological in- volvement via the induction of antigen expression on endothelial cells and the formation of immune complex- es.1 In late stage, organization of basal exudates may strangulate the vessels leading to vascular narrowing and focal weakness.3The common pathological chang- es in cranial blood vessels in tuberculous meningitis are arteritis: Infiltrative, proliferative, necrotizing or fibrinoid necrosis. Vascular involvement starts in adventitia and progressively encroaches to involve the entire vessel wall constituting panarteritis tuberculosa.3 The uncom- mon complications include aneurismal dilatation, mycot- ic aneurysm, thrombus formation and venous sinus thrombosis.2 these different pathological changes prob- ably depend on the type, virulence of Myobacte- rium tuberculosis and on the host immune response to the infection.2
Most of the strokes in TBM are small, multiple, bilateral
and located in the basal ganglia especially the ‘tubercu-
The research paper published by IJSER journal is about Fatal tuberculous meningovasculitis 2
ISSN 2229-5518
lar zone’ which comprises of the caudate, anterior thal- amus, anterior limb and genu of the internal capsule, corresponding to the deep sylvian region.1These are at- tributed to the involvement of medial striate, thala- motuberal and thalamostriate arteries which are em- bedded in exudates and likely to be stretched by a co- existent hydrocephalus. Cortical stroke can also occur due to the involvement of proximal portion of the mid- dle, anterior and posterior cerebral arteries as well as the supraclinoid portion of the internal carotid and basi- lar arteries.2 Small vessel occlusion is common in the early stage of TBM resulting in monoplegia whereas middle cerebral or internal carotid arterial territory in- farcts are common in advance stage resulting in hemi or quadriplegia.2 Vertebrobasilar territory strokes earlier have been reported to be rare but recently 20% of strokes in TBM have been reported in vertebrobasilar territory based on MRI study.2Arteries traversing the sulci of the vertex are usually unaffected.3
TBM related stroke most commonly manifests with in- sidious focal neurological deficit, acute confusional state, meningeal syndrome, headaches, cranial nerve paralysis, coma and seizures. The other neurological manifestations depend on the location of infarctions. A large stroke may result in raised intracranial pressure.2
Tuberculous cerebral vasculitis should be included in the differential diagnosis of any neurological deteriora- tion arising during the course of tuberculous meningi- tis.1
Diffusion weighted imaging (DWI) provides information regarding tissue ischemia at an early stage (within the first hour after stroke) as compared to conventional magnetic resonance imaging (MRI).4 DWI provided in- formation not available on conventional T2 weighted imaging in terms of the multiplicity of lesions and detec- tion of clinically unrelated area in a significant number of patients.4
MRA classically visualizes segmental narrowing, parie- tal irregularities and, sometimes, obstructions. Lep- tomeningeal vessels over the convexities of the brain may be stretched as a result of internal hydrocephalus or brain swelling. Sometimes luxury perfusion with early draining veins may be seen. Although the cerebral vas- culature can be visualized by MRA, direct angiography remains the gold standard for imaging the vascular lu- men.1
Corticosteroids should be prescribed in combination with antituberculous drugs to treat tuberculous meningi- tis.1This regimen were thought to reduce mortality and morbidity but their role in reducing strokes has not been proven. Aspirin also reduces mortality and its role in re- ducing stroke in TBM needs further studies.2
The authors want to thank BAYER S.A for partial fund support.
[1].N.Javaud, S .Certal Rda , J. Stirnemann , AS.Morin , JM.Chamouard , A. Augier , O.Bouchaud , A/Carpentier
, R .Dhote , JL.Dumas , Fantin B, Fain O.Tuberculous cerebral vasculitis: retrospective study of 10 cases. Eur J Intern Med. 2011; 22(6):e99-104.
[2].UK. Misra , J.Kalita , PK.Maurya . Stroke in tubercu- lous meningitis. J Neurol Sci. 201115;303(1-2):22-30.
[3]. J.Kalita J, UK .Misra , PP.Nair . Predictors of stroke and its significance in the outcome of tuberculous men- ingitis. J Stroke Cerebrovasc Dis. 2009;18(4):251-8.
[4]. R.Shukla , A.Abbas , P.Kumar , RK.Gupta , S. Jha, KN.Prasad .Evaluation of cerebral
infarction in tuberculous
meningitis by diffusion weighted imaging.J Infect. 2008;57(4):298-306.
IJSER © 2012
The research paper published by IJSER journal is about Fatal tuberculous meningovasculitis 3
ISSN 2229-5518
IJSER © 2012
The research paper published by IJSER journal is about Fatal tuberculous meningovasculitis 4
ISSN 2229-5518
Oumerzouk Jawad, El Jouehari Abdelhafid, Hssaini, Yahya, Bourazza Ahmed
Neurology department. Military hospital of Rabat. Mo- rocco
Street address: Military hospital. Hay Ryad. Rabat. Mo- rocco
Number and postal code: 10100
Phone number: 00(212)670438897
E-mail: tamamro@yahoo.fr
IJSER © 2012