
International Journal of Scientific & Engineering Research, Volume 6, Issue 2, February-2015 478
ISSN 2229-5518
Design and Implementation of Wireless Sensors Network and Cloud Based Telemedicine System for Rural Clinics and Health Centers
Hafez Fouad, Microelectronics Dept. hafez@eri.sci.eg Hesham Farouk, Computer & Systems Dept. hesham@eri.sci.eg Electronics Research Institute, Cairo, Egypt.
Abstract—Telemedical centers use ICTs to overcome geographical barriers, and increase access to healthcare services. This is particularly beneficial for rural and underserved communities in developing countries – groups that traditionally suffer from lack of access to healthcare. In addition reviewing and discussing the current attempts in wireless body area network technology, a W BAN system that has been designed for healthcare applications will be presented. The wireless system in the W BAN uses medical bands to obtain physiological data from sensor nodes. The medical bands are selected to reduce the interference and thus increase the coexistence of sensor node devices with other network devices available at medical centers. The collected data is transferred to remote stations with a multi-hopping technique using the medical gateway wireless boards. In his paper we propose a complete architecture design and implementation, with real test on site for patient data collection, telemedicine system with mutli-users facilities for both sides, Doctors, patients and medical centers. The system offer the facilities of connecting to telehealth W SN and has two types of dash boards; for patients side and for doctor side with the facilities of displaying in one screen capture the case under supervision from a doctor. The core of the proposed system is based on using web interfaces hosted on cloud environment. We add a big data technology analytical tool to analyze the patient data stored on cloud database to get some information – geographically distributed for example which may help the decision maker for example. It is an effective solution for providing specialty healthcare in the form of improved access and reduced cost to the rural patients and the reduced professional isolation of the rural doctors. Telemedical centers can enable ordinary doctors to perform extra-ordinary tasks. The proposed system got real results applied on Pulse company wearable Mobile ECG device that can make a remote monitoring to the patient using cloud computing.
Index Term—Telemedicine, W ireless sensor network, eHealthcare, Medical Center, Cloud cpmputing, Rural Health Clinics. Health monitoring system.
—————————— ——————————
electronically and the healthcare professional is notified for further action.
ealthcare must be as efficient as possible and provides
an opportunity for the application of telehealth
centers. Information and communication technologies
(ICTs) have great potential to address some of the challenges faced by both developed and developing countries in providing accessible, cost-effective, high-quality healthcare services. Telemedicine, defined by the WHO, World Health
Organization, as "the use of information and communications technology (ICT) to deliver health care particularly in settings where access to medical services is insufficient". The industry can be placed into three basic models as illustrated in Fig.1 [1], which are:
● Store and forward – In this model, data is gathered by the primary care giver, stored electronically and transmitted (securely) to a specialist for review at a different location. This method is used for non-Critical care such as those in dermatology, radiology and pathology.
● Remote Monitoring – In this type of service offering, the company monitors routine data from patients such as ECG, glucose levels and alarming trends are identified, stored
————————————————
• Author Hafez Fouad is a researcher at Electronics Research Institute, EGYPT since 1994, in Microelectronics engineering Dept. His current
research in the field of RFICs, Telemedicine, Wireless Sensors network, and
Bioelectronics PH-00201068808540. E-mail: hafez@eri.sci.eg
• Co-Author Hesham Farouk is an associate Prof. since 2012.He joined the
Electronics Research Institute in 1993. His fields of research, signal
● Interactive Medicine – In such an environment primary care givers can often interact in real – time with experts to consult about a patient’s condition and seek advice on treatment options.
Current Trends:
● US federal government grants have aided the growth of
telemedicine market in the country.
● Europe, on the other hand, has experienced growth because of an aging population and a preference for home based treatments.
● In Asia, the growth in telemedicine is attributable to an aging population, rising health care costs and a wide disparity in quality of health care available in urban and rural areas.
The total world market for telemedicine is expected to reach Rural areas are facing a limited supply of pharmacists, dentists and mental health professionals. Overall, we found that measured performance of rural physicians tended to be lower than performance of physicians in urban or suburban areas. To better understand the health issues facing rural communities, we asked physicians and consumers about their views on the most pressing health challenges in their communities and found that chronic conditions were major concerns for both groups. Telemedicine is defined as the use of telecommunications to provide medical information and services. It may be as simple as two health professionals
processing, Neural Networks, image compression, video processing, pattern IJSER © 2015
recognition and machine vision. PH-00201006087180. E-mail:
hesham@eri.sci.eg
http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 2, February-2015 479
ISSN 2229-5518
discussing a case over the telephone, or as sophisticated as using satellite technology to broadcast a consultation between providers at facilities in two countries, using videoconferencing equipment or robotic technology. 18 billion by 2015
Fig.1. Three Basic Models of Telemedicine
Closely associated with telemedicine is the term "telehealth," which is often used to encompass a broader definition of remote healthcare that does not always involve clinical services. Videoconferencing, transmission of still images, e- health including patient portals, remote monitoring of vital signs, continuing medical education and nursing call centers are all considered part of telemedicine and telehealth. Telemedicine enables a physician or specialist at one site to deliver healthcare, diagnose patients, give intra-operative assistance, provide therapy, or consult with another physician or paramedical personnel at a remote site. Telemedicine system consists of customized medical software integrated with computer hardware, along with medical diagnostic instruments connected to the commercial VSAT (Very Small Aperture Terminal) at each location or fiber optics[2-4].
We focus on the role telemedicine can play in helping clinics expand services in rural areas by connecting patients to specialists. Mobile clinics equipped with new technology can move beyond traditional functions and provide broader range of services. Advances in communications and information technology are transforming medical care by changing the way care is delivered and how people access medical services. One technology driving these improvements is telemedicine: the provision of clinical services using the electronic exchange of medical information, cross-site transmission of digital images and electronic communications (e.g., physician patient email, remote monitoring of vital signs and video patient consults with physicians). Rapidly emerging as a component of telemedicine is medical care that relies on mobile devices such as cellular phones, personal digital assistants and laptops (often referred to as mHealth). High resolution cameras, digital imaging, the use of smart phones and broadband high-speed connections have dramatically improved the scope and scale of telemedicine’s applicability. The concept of telehealth, often used interchangeably with
telemedicine, refers to a broader set of uses of the technology that includes but also extends beyond the delivery of medical care. Telehealth involves using technology to support activities such as remote medical education, health services research and some administrative functions [2,5]. Fig.2 shows the concept of telemedicine in rural locations[6].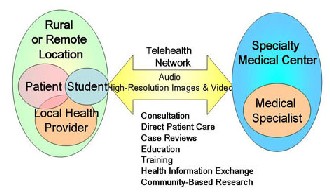
Fig.2. Telemedicine Concept
By diminishing the impact of distance and time, telemedicine can in theory expand capacity, foster coordinated care, improve the quality and efficiency of the delivery system and support more patient self-management. Fig.2 shows the types of telemedicine that are most functional today primarily expand the capacity of the rural health care delivery system, making it easier for patients to be seen and treated, especially by specialists. These types of telemedicine include: automated expert analytic system .
The transmission of images or clinical data from an electronic device to a medical center is known as “store and forward.” Clinical information is “stored” with a patient record and then forwarded to a provider for further review.
Fig.3. Telemedicine Usage in Rural
Dermatologists and radiologists increasingly use this technology as do emergency medical personnel who can transfer medical information and images from ambulances to hospital emergency rooms [7]. Store and forward technology, shown in Fig.3, also supports ongoing remote patient
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 2, February-2015 480
ISSN 2229-5518
monitoring and management of key medical indicators (e.g., blood glucose levels) in patients with chronic illness.
These consultations, commonly conducted over the Internet using secure live connections and Web cams, can either substitute for in-person visits or support care between appointments. Audio and online approaches may also be used. In rural areas, video consultations extend the reach of scarce specialists; some federally qualified health centers use video technology for this purpose. The interactive capabilities provided by video also support the technology’s use in behavioral health care; federal veterans hospitals use telemedicine to facilitate treatment for Post-Traumatic Stress Disorder. Online care is well-suited to conditions where a one-on-one consult could result in a quick diagnosis, such as respiratory infections, urinary tract infections, acute conjunctivitis and hypertension. Current technology allows patients to connect to more than one provider at a time: a primary care physician can join with a specialist, for example, to confer with a patient. If physicians and patients are not available at the same time, either one can prepare a video report that can be accessed at a later time by the other [3].
1.5 Support for patients managing their own health. Patients can use the Internet to obtain specialized health information and to access online discussion groups for peer-
to-peer support. Surveys show that patients are often willing
to manage their personal health information over smart
phones and are interested in pursuing other types of care
delivery via mobile devices [8]. Phones now have the ability
to store health information like immunizations and prescriptions. When connected to portable medical devices, phones can capture blood glucose levels, blood pressure values and vitals, and transfer information to personal health records. These tools help people address their health and wellness needs through online care management and wellness programs that teach positive long-term behavior change.
1.6 Remote monitoring.
Providers use remote monitoring to track changes in important patient vital signs such as weight, body temperature, blood pressure and heart rhythms. Patients wear monitors or use devices such as scales located in their own homes but connected to their physicians’ offices, making it possible to monitor a patient’s health without an office visit. This remote monitoring supports the early detection of possible health problems (for example, patients with congestive heart failure who suddenly gain weight may be retaining water, a sign of decreased heart function that can be treated with medication). Pharmacists may use information from remote monitoring to counsel patients on the effective and safe use of medications [9].
1.7 Intensive care unit (ICU) telemonitoring (e-ICUs).
These programs extend the reach of critical care providers.
Specialist physicians and critical care nurses staff round-the- clock tele-ICU centers (or tele-hubs) that receive data from monitoring devices tracking patients in ICUs in small hospitals, including those in rural areas. The ICU specialists in the tele-hub can support the care given on-site by providers who may have less critical care expertise.
Remote, rural clinics may not be able to provide a full-scale pharmacy, but access to an electronic connection to a pharmacy and a pharmacist can help patients receive both medications and medication counseling (ultimately improving medication compliance). By connecting pharmacies at urban hospitals to small rural hospitals, pharmacists can guide dispensing technicians to fill prescriptions [3]. In some cases, however, legal requirements that pharmacists be present for the dispensing of medication may complicate this practice [10].
1-Tele-consultation room
2-Patient engagement facilities (bed, scopes, etc.
3-Selective medical and medico-IT equipment’s, preferably IT
compatible, with interface to Telemedicine and/or other software /
hardware
4-Computer hardware / software platform (PC, switch, etc.) and IT
electronics equipment [11]
Fig.4 Requirements in Medical Centers
1. Mobile vans are a part of telemedicine service
2. Desktop PC platform with Laser Print
3. IP Video Conferencing Kit
4. Tele medicine software
5. Digital ECG
6. A3 Film Scanner
7. Digital Microscope & Camera
8. Glucometer & Haemogram analyzer
9. Non-invasive Pulse & Blood Pressure unit
10. Connectivity device & Router
Looking to the past experience for success of telemedicine:
11. Video conferencing
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 2, February-2015 481
ISSN 2229-5518
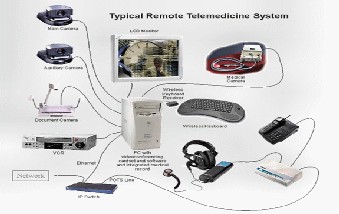
12. Accompanied by data and image transfer (live
13. Common software usage at both ends, thus globalization of a single database software
14. Role of trained technical personnel is equally important and necessary at the patient end.
15. Successful remuneration system to attract private practitioners
The Centers for Medicare and Medicaid Services (CMS) define the distant site as the telehealth site where the provider/specialist is seeing the patient at a distance or consulting with a patient’s provider. Others common names
for this term include – hub site, specialty site, provider/physician site and referral site. Fig. (5-a).
A digital camera is typically used to take still images of a patient. General uses for this type of camera include dermatology and wound care. This camera produces images that can be downloaded to a PC and sent to a provider/consultant over a network.
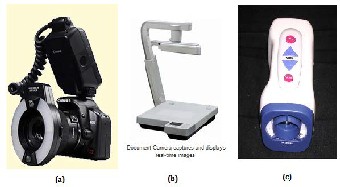
A camera that can display written or typed information (e.g., lab results), photographs, graphics (e.g., EKG strips) and in some cases X-Rays. Figure (5-b).
Fig.5 (a) Digital Camera (b) Document Camera (c) Patient Exam Camera
This is the camera typically used to examine the general condition of the patient. Types of cameras include those that may be embedded with set-top videoconferencing units, handheld video cameras, gooseneck cameras, camcorders, etc. The camera may be analog or digital depending upon the connection to the videoconferencing unit. Fig.5-c [12-16] and Fig 6 [17,18].
Fig.6 Telemedicine Facilities
The proposed system will have many advantages which are:
1. Patient dashboard:
Which is an online board having up to date status of the patient and the doctor diagnoses updates and sensors reading updates and accept clinical manual update as well, Fig.7 represent a screen shot sample for a patient data on the dashboard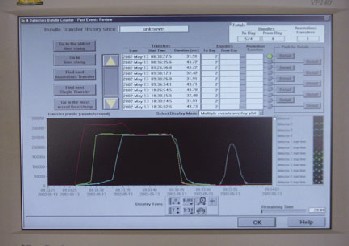
Fig.7 screenshot for patient data on the dashboard
2. Doctor Dash board:
Which will enable the doctor the follow up and update the diagnoses process for the group of patient he follow up. Fig 8 give a sample of a screen shot to the doctor dash board which display online the cases under this doctor supervision
3. Many to many system connectivity:
By meaning the system will enable many doctors to access the system for same patient dashboard at the same time.
4. The analytical layer:
Which will process the accumulated data stored on the cloud database and extract features of diseases on geographical base for example
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 2, February-2015 482
ISSN 2229-5518
The proposed system will be composed of 3 verticals and equipped to work online (as video conferencing option) or offline as just reading the patient record by doctor Figure – represents the proposed system verticals:
1) Telemedicine WSN sets (wearable sensors)
2) Technical Medical Center components(Website – Cloud Environment- dash boards (patient and doctors) – Big data analytic tool)
3) Doctors sets (Application interface)
Which is a group of Health WSN as Temperature, Pleasure,
Heart rate, Glucose level etc.
These sensors are able to connect to internet through direct connections or through mobile application after applying the required data gathering for any patient, the data will be transmitted through the internet, Bluetooth to a portable computer connected to the central private cloud built through a registered login account for that patient to save the log data file on the telemedicine system
Fig.8 A screen shot sample for the doctor dash board
a) Website : We already developed a tailored web site dedicated to the function of patients and doctors registration with accessing the cloud database
b) Cloud Environment
c) Electronics Research Institute (ERI) recently established
and developed a cloud environment in its Cairo campus
with a disaster recovery site in the research city in
Alexandria. The proposed system will deployed and
tested on this environment [19-20]
d) Big data analytic tool
e) A higher level layer will be added to the system which is apply an analytical tools on the already saved patients records which will enable the decision makers to analyze the diseases geographical pattern for example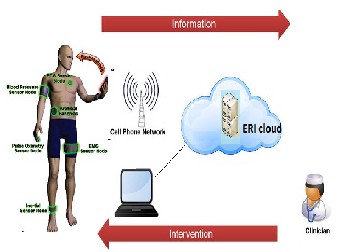
Fig.9: Proposed system architecture
This is the doctor side which is mainly the application interface which will enable the doctor to read the patient records and enable him to make a video conference with him on the other side if required
Fig.10: Patient process cycle
Fig.11: Doctor Process cycle
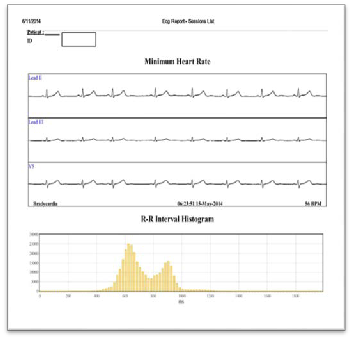
The proposed system was tested on Wearable sensor product from PULSE Company for wearable Mobile ECG device that can make a remote monitoring to the patient using cloud computing. Sample from the generated reports was displayed in Fig 12 and the device used is presented in Fig13
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 2, February-2015 483
ISSN 2229-5518
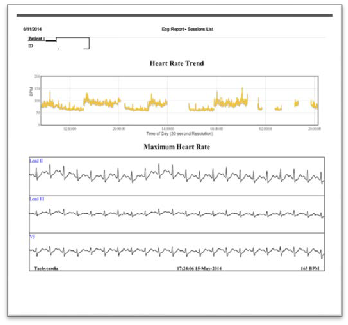

Fig13 Pulse Company Wearable device
(a)
(b)
Fig. 12 (a,b) represent the graph from the real test applied by the
proposed system on PULSE wearable product
The Proposed system of Remote Healthcare monitoring center for Telemedicine system through web-Portal is achieved and running. The equipped system with new technology is used to provide wide range of services in Telemedical center which facilitates the provision of medical aids from a distance. Many features are proposed as dash board for patients and doctors. It is an effective solution for providing specialty healthcare in the form of improved access and reduced cost to the rural patients and the reduced professional isolation of the rural doctors. Telemedical centers can enable ordinary doctors to perform extra-ordinary tasks. While some forms of telemedicine, such as store and forward applications for imaging reads, are commonly in use, other uses of the technology are still in developing. Among rural hospitals, about one-fourth participated in tele-cardiology and video teleconferencing for consultations and about 10 percent used tele-emergency services. Steady growth is occurring with e-ICU hubs and their use is increasing in small critical care hospitals.
Other telemedicine technologies hold promise for the future, although their full realization may be some way off, these include:
• Telehealth services. This approach to telemedicine uses cloud computing — servers hosted on the Internet — to allow providers to connect with systems from different organizations and share health data generated from patients remotely. It can, for example, link remote health monitoring, electronic health records and services such as
24-hour call centers. This approach removes the burden of
having to invest in telemedicine infrastructure and
distributes costs among multiple parties.
• Robotics. Telemedicine robots allow doctors to travel
virtually to a patient’s bedside. Robots are also beginning to
IJSER © 2015 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 6, Issue 2, February-2015 484
ISSN 2229-5518
be used in remote surgery, although most robotic surgery is still carried out by on-site surgeons.
• Clinical kiosks. These care sites may become a tool to bring medical care directly to patients and help increase access in areas with limited broadband connectivity. When fully realized, clinical kiosks should be capable of taking biometric readings and allowing individuals to upload vital signs with the eventual aim of providing a full diagnostic evaluation and recommendations for treatment without the use of on-site personnel.
The authors are highly express the great thanks to Pulse company team www.pulse-eg.com through availing their innovative product as a wearable sensor to measure the vital value for patient which enable this research and the suggested model explained through, to have a practical test cases.
[1] Moshaddique Al Ameen & Jingwei Liu&Kyungsup Kwak, "Security and Privacy Issues in Wireless Sensor Networks for Healthcare Applications", Journal of Medical Systems Mar, 2012, http://link.springer.com/search?query=Security+and+Privacy+Issues+in+ Wireless+Sensor+Networks+for+Healthcare+Applications
[2] Hafez Fouad, “ Continuous Health-monitoring for early Detection of Patient by Web Telemedicine System “, International Conference on Circuits, Systems and Signal Processing , Saint Petersburg State Politechnical University, Russia, Sep,23-25, 2014. 2014
[3] Chin-Feng Lin, and Ching Yi-Li, "A DS UWB Transmission System for Wireless Telemedicine," WSEAS TRANSACTIONS on SYSTEMS, Issue 7, Volume 7, July 2008.
[4] Hafez Fouad, Hesham Farouk, " Design and Implementation of Video Conferencing Cloud-based Network using VoIP for Remote Health Monitoring in Telemedicine System", International Journal of Computer Informatics & Technological Engineering IJCITE, INDIA, Vol:1, Mar-April
2014.
[5] Hafez Fouad, “ Patient-oriented Web Telemedicine system For Health Monitoring ", Journal of Communication and Computer, CA 91745, USA,Vol.11, Issue 2, pp-168-178, Feb., 2014.
[6] Hafez Fouad," Web-based Medical Informatics to support Telemedicine System", International Journal of Engineering & Computer Science IJECS- IJENS, Vol:14, No:01, Feb, 2014.
[7] Hafez Fouad, Haythem Abdullah, " ICT-based Telemedicine for the Egyptian
Society," The Second International Conference on Information Technology
Convergence and Services, India, ITCSE 2013.
[8] U.S. Department of Health and Human Services and Services Administration Bureau of Health Professionals (2000). The Pharmacist Workforce: A Study of the Supply and Demand for Pharmacists.
[9] Sarasohn-Kahn J (2011). The Connected Patient: Charting the Vital Signs of
Remote Health Monitoring, California Health Care Foundation.
[10] American Telemedicine Association (2007). Telehealth and Health Care
Provider Shortages. American telemedicine Association Position Statement.
[11] Edwards J, et al (2009). Hype Cycle for Telemedicine, Gartner Industry
Research. Publication G00169011.
[12] Bergmo TS (2010). Economic Evaluation in Telemedicine – Still Room for
Improvement, J Telemed Telecare 16.5 (2010): 229-31. DOI:
10.1258/jtt.2010.009008.
[13] American Telemedicine Association (2007). Telehealth and Health Care
Provider Shortages. American telemedicine Association Position Statement.
[14] Young LB, et al (2011). Impact of Telemedicine Intensive Care Unit Coverage on Patient Outcomes: A Systematic Review and Meta-analysis, Arch Intern Med 171.6: 498-506. oi:10.1001/archinternmed.2011.61.
[15] Agency for Health Research and Quality (2006). Telemedicine for the
Medicare Population: Update. AHRQ Publication No. 06-E007.
[16] U.S. Veterans Administration (2010). U.S. Veterans Administration Brochure
Series, Rural Health, 2010.
[17] Berenson RA, Grossman JM and November EA (2009). Does Telemonitoring of Patients – the eICU – Improve Intensive Care? Health Affairs, 28.5: w937 – w947. DOI: 10.1377/hlthaff.28.5.w937.
[18] McConnochie KM, et al (2009). Acute Illness Care Patterns Change with Use
of Telemedicine, Pediatrics 123.6: e989 – e995. DOI: 10.1542/peds.2008-2698). [19] Jui-chien Hsieh* and Meng- Wei Hsu,”A cloud computing based 12-lead
ECG telemedicine service”, BMC Medical Informatics and Decision Making 2012,
12:77.
[20] Jordi Vilaplana et al,” The cloud paradigm applied to e-Health”, BMC Medical
Informatics and Decision Making 2013, 13:35.
Hafez Fouad, has received his BSc. degree in Electronics and communications engineering in 1993, EGYPT and received his M.Sc. and Ph.D. degrees from Ain Shams University in Cairo, 2001 and 2008. His Ph.D. is dedicated to Performance Optimization of CMOS RF Power Amplifiers for Mobile Communication systems. The M.Sc. is dedicated to Design and Optimization of Silicon RF Front-ends For Mobile Communication Systems. He is assistant Professor at Electronics Research Institute (ERI), Ministry of Scientific Research since 1994, Cairo, Egypt. His current research interests are Telemedicine Systems, wireless sensors network, Bioelectronics, Bioinformatics and their applications.
Hesham Farouk is an associate Prof. since 2012.He joined the Electronics Research Institute, Egypt, in 1993. His fields of research are signal processing, mobile systems, Neural Networks, image compression, video processing, video compression, video indexing and retrieval, video on demand, pattern recognition and machine vision. Dr. Farouk received his Ph.D. at 2001 from Electronics & Communications Dept., Faculty of Engineering, Cairo Univ. and his M.Sc. at 1996 from Electronics & Communications Dept., Faculty of Engineering, Cairo Univ. Acting Manager Mobile, Social and Cloud Network Competence Center(MSCC) | Ministry of Communication and Information Technology.
IJSER © 2015 http://www.ijser.org