International Journal of Scientific & Engineering Research, Volume 4, Issue 12, December-2013 1386
ISSN 2229-5518
ANTIMICROBIAL SUSCEPTIBILITY TESTING OF CIPROFLOXACIN & CEFEPIME AGAINST STAPHYLOCOCCUS AUREUS & ESCHERICHIA COLI
Tuba Siddiqui*, Baqir S.Naqvi**, Nausheen Alam*, Lubna Bashir*, Shazia Naz*, Ghazala Naqvi*, Mirza Taswar Baig*.Sabiha
Tasleem*
*Department of Pharmaceutical Sciences, Faculty of Pharmacy, Federal Urdu University of Arts, Sciences and Technology, Gulshan-e- Iqbal, Karachi-75300, Pakistan, *Department of Pharmacology, Faculty of Pharmacy, University of Karachi-75270, Pakistan.
** Department of Pharmaceutical Sciences, Faculty of Pharmacy, University of Karachi- 75270, Pakistan.
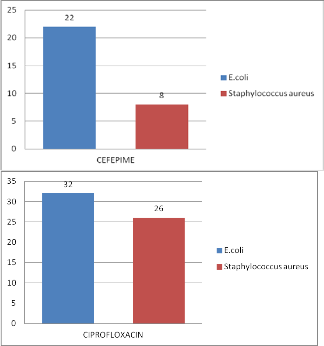
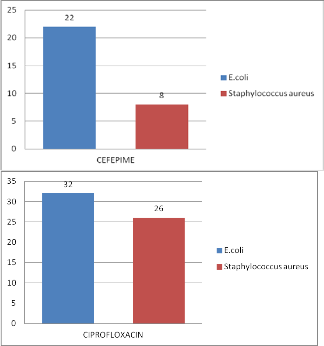
Abstract— Excessive and Discriminate usage of antibiotics is the major cause of microbal resistance to the majority of antimicrobial agents is a serious and global problem On the other hand high prevalence of drug resistance bacteria in the indigenous focal flora, lack of education poor stand- ards of sanitation and prevalaence of malnutrition are the other contributing factors. This problem is at its extreme in developing countries like Pakistan. Therefore the development of the survilance program at National level is one of the most effective ways to control antibiotic resistance .To accomplish this task fifty clinical isolates of each of Staphylococcus aureus and Escherichia coli were collected from different hospitals and pathological laboratories in Karachi. These isolates were evaluated against Ciprotloxacin and Cefepime to investigate their susceptibility. The anti bacterial activity of Ciprofloxa- cin and Cefepime was carried out by disc diffusion method. Ciprofloxacin is 74 % and 68% sensitive to Staphylococcus aureus and Escherichia coli and shows 26% and 32% resistance respectively. Cefepime is 92% and 78% sensitive to Staphylococcus aureus and Escherichia coli and shows 8% and
22% resistance respectively. Hence it has been evaluated that all these clinical isolates have developed resistance to Ciprofloxacin and Cefepime. So that present study reinforce the adherenc to antibiotic control policy and regular susceptibility testing to tackle the problem of anti-micobial resistance.
Index Terms— Antimicrobials, cefepime, ciprofloxacin, Escherichia Coli, Staphylococcus Aureus, susceptibility testing, resistance.
—————————— ——————————
ESISTANCE to antimicrobial agents is a major and crushed issue from more than fifty years and considered
as root cause of increased morbidity, mortality and health care cost. Inappropriate use of antibiotics is considered the major contributing factor; as well as, poor implementation of infection control measures, prolonged hospitalization, use of invasive procedures and admission to intensive care units the are other contributing factors. [1]
Predominent cause of nosocomial and community- acquired infections are Gram positive cocci such as Staphylo- coccus aureus. These organisms have ability to acquire re- sistance rapidly to frequently used drugs through selective pressure of environemnt and via the genetic evolution of bac- teria [1]. Gram negative bacteria such as Escherichia coli ac- quire resistance to antibiotics as the result of gene mutation. [2]
Antibiotic resistance is considered to be direct conse- quence of antibiotic use in humans. Quinolones are broad-
spectrum, bactericidal antibacterial agent have potent activity, even against intracellular pathogens, and ease of administra- tion (oral, parenteral), has firmly established them both in the hospital and the community.The emergence of resistance is the natural response of microbes to the presence of antimicrobials, and it is generally accepted that the greater the consucmptions of antimicrobials,the greater will be the emergence of antimi- crobial resistance [3]. Gram-positive and Gram-negative bacte- ria have been reported to be resistant to Quinolones. Three mechanisms of resistance have been established with Quin- olones: alterations in target of Quinolones, bacterial cell per- meability, and drug efflux mechanisms [4]. Plasmid-mediated resistance was also reported but its appears to be very rare compared with chromosomally mediated mechanisms of changes caused by point mutation in genes which are consid- ered as the single major cause of resistance to Quinolones [5].
Cefepime is relatively new cephalosporin wth an extended spectrum of antibacterial activity that includes both aerobic Gram (-) and Gram (+) bacteria. The mechanism of
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 12, December-2013 1387
ISSN 2229-5518
resistance to cephalosporin is the destruction of the cephalo- sporin by hydrolysis of the βlactams ring. Many Gram- positive micro organisms release relatively large amount βlac- tamase into the surrounding medium .Although Gram- nega- tive bacteria seems to produce less βlactamase; the location of their enzyme in the preplasmic space may make it more effec- tive in destroying cephalosporin as they diffuse to their target on the inner membrane. [6]
of Staphylococcus aureus and 68% Escherichia coli are sus- ceptable to Ciprofloxacin.
92% clinical isolates of Staphylococcus aureus and
78% Escherichia coli are susceptable to Cefepime.
A total of one hundred clinical isolates of Staphylo- coccus aureus and Escherichia coli were collected for culture and sensitivity from different hospitals and pathological la-
boratories in Karachi. After identification were cultured on
slants containing Muller Hinton agar and stored at temp 2-4
°C. Before testing, isolates were brought to room temp. Mueller Hinton medium ﴾Difco, Detroit,USA﴿ was used to culture the islolate and identified by conventional techniques (Forbes BA). Antibiotic sensitvity test was done by Kirby Baeur disk difussion method.
Briefly
• Clinical isolates and the control strains were brought to room temperature and were cultured in Mueller Hinton broth tubes at 37°C for 2-4 hours so that, tur- bidity could be matched to Macfarland No 0.5 stand- ard.
• Muller Hinton agar plates for cultured sensitivity
were dried and labeled.
• Muller Hinton agar plates were seeded with test or-
ganism using sterile cotton swab.
• Disk of different antibiotic were then placed on agar
using asterile forcep.
• Petri plates were incubated for 24 hours at 37°C prior
to determination of result.
• A vernier caliper was used to measure the zone of in- hibition. The zone diameter of each antibiotic disc was interpreted using criteria published by National Committee for Clinical Laboratory Standards USA (NCCLS).
The present study one hundred clinical isolates of Staphylococcus aureus and Escherichia coli. The isolates were collected from different pathological labs and hospital in Ka- rachi and sensitivity pattern of determine by Kirby Baure Method as in Table No.1 and Graph No. 1 & 2.
The present study showed that 74% clinical isolates
Fig 1&2 Percent resistance of Ciprofloxacin and Cefepime
Antimicrobial | Bacterial organism | Isloates (n) | % Suscepta- ble | % Re- sistance |
Ciprofloxacin | E.coli | 50 | 68 | 32 |
Ciprofloxacin | Staphylococcus aureus | 50 | 74 | 26 |
Cefepime | E.coli | 50 | 78 | 22 |
Staphylococcus aureus | 50 | 92 | 8 |
This study was conducted to findout the resistance pattern of Ciprofloxacin and Cefepime using E.coli and S.aureus to generate data regarding the antibiotic sensitivity pattern of these isolates. So that initiation of empirical thera-
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 12, December-2013 1388
ISSN 2229-5518
py could be made more effective in infection caused by these
isolates.
In the present study 32% clinical isolates of Esche- richia coli were resistant to Ciprofloxacin
Low sensitivities of Escherichia coli was observed in this study is consistent with the earlier work. Eksi and coworkers in 2007 reported 35.8% resistance to E.coli.
.AbdulRehman and coworkers in 2010 reported a gradual increase in resistance from year 2002 to2005 in most of gram negative isolates[7,8] .For E.coli resistance rate were 23.85% in 2002 to 33.1% in 2005. Although this high resistance of Escherichia coli to Ciprofloxacin was reported in our study, enhanced susceptibility had been reported by previous workers. Lauderdale in Taiwan reported 12% resistance to Ciprofloxacin[9]. Similarly (Richard et. al 2003) reported
19.5% resistance in Spain and 6% resistance in France in
2000-2001. [10]
The 26%resistance of Ciprofloxacin to Staphylococ-
Although low sensitivity of Escherichia coli
78% to Cefepime as observed in this study, enhanced
susceptibilities had been observed by previous report-
ers. Douglas in 1999 reported susceptibility 97.5- 100.0
% to E.coli. Further, prio researchers Lewis in 1998 and
Douglas in 1999 reported 91.7 % and 97.8% susceptibil-
ity of Cefepime to Escherichia coli. This difference can be attributed to the variation of resistance patterns to antimicrobials based on their usage.[17]
The encouraging finding in our study was the low percentage resistance to Cefepime. However, caution is required; the use of flu- roquinolone drugs must be restrictive and discriminative so as to prevent a rapid development of drug resistance. Our study highlights the need for antimicrobial suscep- tibility pattern determination from time to time so that proper guidelines for hospital antibiotics policies can be developed. Hence this present study will be very useful for the pharmacist and physician
IJSER
cus aureus as recorded in this work is in conformity with
finding of of (Baqir et. al 2002) in which 26% Ciprofloxacin
resistant Staphylococcus aureus was reported in strong agreement with published reports. [11,12,13] This finding was however different with the work of (Zhang et. al 2002) who reported 62.2% resistance.[14]
4.2 CEFEPIME
Ninety two percent (92%) clinical isolates of Staphylo- coccus aureus and seventy eight percent 78% of Esche- richia coli are susceptible to Cefepime.
The result of this study indicated that Cefepime had highest sensitivity 92% to Staphylococ- cus aureus. This apparently high level of sensitivity to cefepime appears to suggest that Cefepime could be a drug of choice for treating infections caused by Staphy- lococcus aureus in the study area .This findings is con- sistent with previous reports .For instance, 100% sus- ceptibility of Cefepime to Staphylococcus aureus has been reported . Sader in 2005 and Tallis in1999 reported
100% In addition, high sensitivities of Cefepime against
methicillin sensitive Stapylococci was also highlight-
————————————————
• Corresponding author: Nausheen Alam is currently pursuing Ph.D in Pharmacology in University of Karachi, Pakistan, PH-+92 321 2606400. E-mail: (N. Alam) Nausheenasarosh@hotmail.com
ened by Douglas 1999. [15, 16]
for prescribing antimicrobial drug.
[1] Jocelyn Y. Ang, Elias Ezike and Basim 1. Asmar Vol- ume 71, Number 3 / March', 2004 Antibacterial resistance Indian Journal of Pediatrics
[2] Siu LK (2002)Antibiotics : action and resistance in
Gram-negative bacteria J Microbiol Immunol Infect .351-11.
[3] Williams R (2001). Resistance as a world wide prob- lem. In: Lewis K, Slayers AA, Tabers HW and Wax RG (ed) bacterial resistance to antimicrobials. Marcel and Dekker Inc., New York, pp. 249-256
[4] Bearden DT and Danziger LH (2001). Mechanism of Action and Resistance to Quinlones. Pharma- cotherapy. 21(10): 224-232
[5] Fish DN (2001. Gatifloxacin: An Advanced 8-methoxy
Fluroquinolone Pharmacotherapy. 21(1): 35-59
[6] Louis Sanford Goodman ,Lee E ,Limbird ,Perry B,Millinof ,Raymond W. Ruddon ,Alfred Goodman Gilman ,Joel G.Hardman(1996). Goodman and Gil-
man,s. The Pharmacological basis of Therapeutics
.Ninth Edition pp 1 029- 1096.
[7] Eksi F, Ozer G. Investigation of the frequency of extend- ed spectrum beta- Iactamases and antibiotic resistance in clinical isolates of Escherichia coli and Klebsiella sp. Balci IMikrobiyol Bul. 2007 Jul;41(3):447-52.
IJSER © 2013 http://www.ijser.org
International Journal of Scientific & Engineering Research, Volume 4, Issue 12, December-2013 1389
ISSN 2229-5518
[8] Abdul Rehman Muhammad Al Quresh, Muhammad Ab- dul Tawaibah. Invitro Ciprofloxacin resistance profile among gram –ve bacteria isolated from clinical specimens in a teaching hospital
[9] Lauderdale TL, Clifford McDonald L, Shiau YR, Chen PC, Wang HY, LaiJF, Ho M. (2004). The status of anti- microbial resistance in Taiwan among Gram-negative pathogens: the Taiwan surveillance of antimicrobial re- sistance (TSAR) program, 2000. Diagn Microbiol Infect Dis. 48(3):211-9.
[10]Richard P. Wenzel, Daniel F. Sahm, Clyde Thornsberry, Deborah C. Draghi, Mark E. Jones, and James A. Kar- lowsky.In Vitro Susceptibilities of Gram- Negative Bacte- ria Isolated from Hospitalized Patients in Four European Countries, Canada, and the United States in 2000-200 I to Expanded-Spectrum Cephalosporins and Comparator An- timicrobials: Implications for Therapy. Antimicrobial Agents and Chemotherapy, October 2003, p. 3089-3098, Vol. 47, No. 10
[11]Baqir S Naqvi ,Masroor Ahmed .Muhamrnad Harris Shoaib, Dilnawaz Shaikh , Khursheed Hashmi (2002) . Comparative antimicrobial evaluation of Cephalosporins and Quinolones in common Pediatric Infections. Pakistan
(1998). Diagn Microbiol Infect Dis. 2000
May;37(1):63-74.
J Pharmaceut Sci. 15(2): 13-20
[12]Baum SE, Morris JT, Dooley DP, Watson R. Methicillin- resistant Staphylococcus aureus in an adult military beneficiary population lacking risk factors: susceptibility to orally available agents. Mil Med. 2003 Feb;168(2):
126-30.
[13]Marangon FB, Miller D. Muallem MS, Romano AC, Al- fonso EC. (2004). Ciprofloxacin and levofloxacin re- sistance among methicillin-sensitive Staphylococcus au- reus isolates from keratitis and conjuctivis. Am ] Opthal- mol. 137(3):453-8.
[14]Zhang YL, Geng SN, Lai FC , Wang NP.(2002) Survey on drug resistance to ciprofloxacin in common pathogenic bacteria. Oi Yi Jun Yi Da Xue Xue Bao 22(4):378-9.
[15]Sader HS ,Fritsche TR, Jones RN (2005). Potency and spectrum trends for cefepime tested against 65746 clin- ical bacterial isolates collected in North American med- ical centers: result from the SENTRY Antimicrobial Surveillances Program .Diagn Microbiol Infect Dis
.52(3):265-73.(1998- 2003)
[16]Tallis E ,Rudensky B, Attitas D, Raveh D, Schlesinger Y, Yinnon AM (1999). Invitro activity of cefepime and other broad spectrum antimicrobials against several groups of Gram negative bacilli and Staphylococcus aureus .Diagn Microbiol Infect Dis .35(4):317-23.
[17]Lewis MT, Gales AC, Sader HS, Pfaller MA, Jones RN. Frequency of occurrence and antimicrobial suscep- tibility patterns for pathogens isolated from latin amer- ican patients with a diagnosis of pneumonia: results from the SENTRY antimicrobial surveillance program
IJSER © 2013 http://www.ijser.org